Paper:
Adapting Balance Training by Changing the Direction of the Tensile Load on the Lumbar Region
Tetsuro Miyazaki*, Takuro Aoki*, Junya Aizawa**, Toshihiro Kawase***, Maina Sogabe*, and Kenji Kawashima*
*Department of Information Physics and Computing, The University of Tokyo
7-3-1 Hongo, Bunkyo-ku, Tokyo 113-8656, Japan
**Faculty of Health Science, Juntendo University
2-1-1 Hongo, Bunkyo-ku, Tokyo 113-8421, Japan
***Department of Information and Communication Engineering, School of Engineering, Tokyo Denki University
5 Senju Asahi-cho, Adachi-ku, Tokyo 120-8551, Japan
In this study, we investigated trainees’ adaptation by conducting static balance training in a tandem standing posture. The horizontal tensile force loads in the front, back, left, and right directions were applied using pneumatic artificial muscles. We analyzed the adaptation that occurred during training by changing the direction of the horizontal tensile load on the lumbar region according to the tendency of the trainee. We conducted the experiments using the following protocol. Ten trainees participated in the experiment. In Phase 1, we applied loads in four directions the same number of times in random order to investigate the weak direction in the balance of each trainee. In Phase 2, we measured five trainees in each group: Group 1 was trained in the same way as Phase 1, and Group 2 was intensively trained in two directions in which the balance found in Phase 1 was difficult to maintain. In Phase 3, we performed the same experiment as in Phase 1. We analyzed the adaptation of the trainees using the margin of stability (MoS), a balance evaluation index. We compared the experimental results of Phases 1 and 3. In Group 1, the tendency for improvement in balance was unclear. On the other hand, the balance index in Group 2 improved in four out of five trainees in both the front-back and left-right directions. These results suggest that the training method concentrating on the weak direction could provide a clear directionality to the training effect.
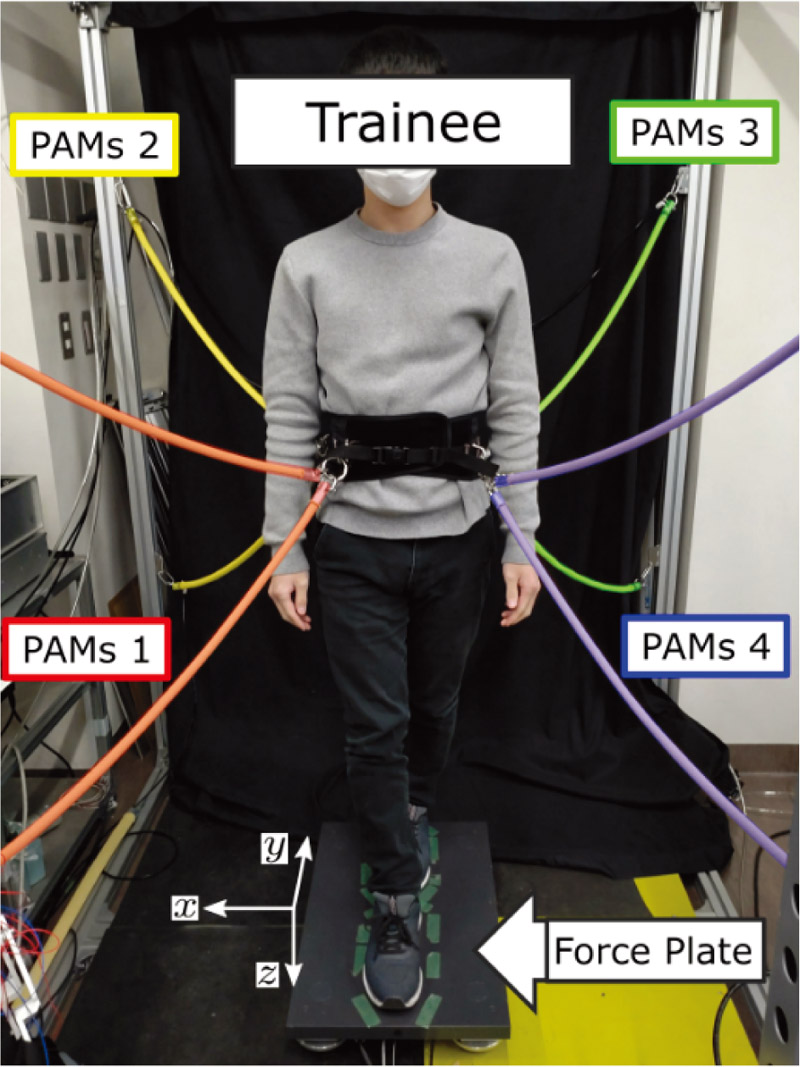
Whole-body training device using PAMs
- [1] S. D. Berry and R. Miller, “Falls: epidemiology, pathophysiology, and relationship to fracture,” Current Osteoporosis Reports, Vol.6, No.4, pp. 149-154, doi: 10.1007/s11914-008-0026-4, 2008.
- [2] M. M. Madureira, L. Takayama, A. L. Gallinaro, V. F. Caparbo, R. A. Costa, and R. M. R. Pereira, “Balance training program is highly effective in improving functional status and reducing the risk of falls in elderly women with osteoporosis: a randomized controlled trial,” Osteoporos, Vol.18, No.4, pp. 419-425, doi: 10.1007/s00198-006-0252-5, 2007.
- [3] S. Morrison, S. R. Colberg, M. Mariano, H. K. Parson, and A. I. Vinik, “Balance training reduces falls risk in older individuals with type 2 diabetes,” Diabetes Care, Vol.33, No.4, pp. 748-750, doi: 10.2337/dc09-1699, 2010.
- [4] K. Berg, S. Wood-Dauphinée, J. I. Williams, and D. Gayton, “Measuring balance in the elderly: preliminary development of an instrument,” Physiotherapy Canada, Vol.41, pp. 304-311, doi: 10.3138/ptc.41.6.304, 1989.
- [5] F. E. Huxham, P. A. Goldie, and A. E. Patla, “Theoretical considerations in balance assessment,” Australian J. of Physiotherapy, Vol.47, pp. 89-100, doi: 10.1016/s0004-9514(14)60300-7, 2001.
- [6] A. Mansfield, J. S. Wong, J. Bryce, S. Knorr, and K. K. Patterson, “Does perturbation-based balance training prevent falls? Systematic review and meta-analysis of preliminary randomized controlled trials,” Physical Therapy, Vol.95, No.5, pp. 700-709, doi: 10.2522/ptj.20140090, 2015.
- [7] A. Mansfield, A. L. Peters, B. A. Liu, and B. E. Maki, “Effect of a perturbation-based balance training program on compensatory stepping and grasping reactions in older adults: a randomized controlled trial,” Physical Therapy, Vol.90, No.4, pp. 476-491, doi: 10.2522/ptj.20090070, 2010.
- [8] Y. C. Pai, T. Bhatt, F. Yang, and E. Wang, “Perturbation training can reduce community-dwelling older adults’ annual fall risk: a randomized controlled trial,” J. Gerontol. A Biol. Sci. Med. Sci., Vol.69, No.12, pp. 1586-1594, doi: 10.1093/gerona/glu087, 2014.
- [9] E. J. Protas, K. Mitchell, A. Williams, H. Qureshy, K. Caroline, and E. C. Lai, “Gait and step training to reduce falls in Parkinson’s disease,” NeuroRehabilitation, Vol.20, pp. 183-190, doi: 10.3233/NRE-2005-20305, 2005.
- [10] H. Shimada, S. Obuchi, T. Furuna, and T. Suzuki, “New intervention program for preventing falls among frail elderly people: the effects of perturbed walking exercise using a bilateral separated treadmill,” American J. of Physical Medicine and Rehabilitation, Vol.83, pp. 493-499, doi: 10.1097/01.phm.0000130025.54168.91, 2004.
- [11] J. W. Streepey, R. V. Kenyon, and E. A. Keshner, “Visual motion combined with base of support width reveals variable field dependency in healthy young adults,” Exp. Brain. Res., Vol.176, pp. 182-187, doi: 10.1007/s00221-006-0677-2, 2007.
- [12] Y. C. Pai, M. W. Rogers, J. Patton, T. D. Cain, and T. A. Hanke, “Static versus dynamic predictions of protective stepping following waist-pull perturbations in young and older adults,” J. of Biomechanics, Vol.31, pp. 1111-1118, doi: 10.1016/s0021-9290(98)00124-9, 1998.
- [13] D. Martelli, V. Vashista, S. Micera, and S. K. Agrawal, “Direction-dependent adaptation of dynamic gait stability following waist-pull perturbations,” IEEE Trans. on Neural Systems and Rehabilitation Engineering, Vol.24, No.12, pp. 1304-1313, doi: 10.1109/TNSRE.2015.2500100, 2016.
- [14] V. Vashista, X. Jin, and S. K. Agrawal, “Active tethered pelvic assist device (A-TPAD) to study force adaptation in human walking,” IEEE Int. Conf. on Robotics and Automation, pp. 718-723, doi: 10.1109/ICRA.2014.6906933, 2014.
- [15] S. Ito, T. Miyazaki, J. Aizawa, T. Kawase, M. Sogabe, T. Kanno, Y. Nakajima, and K. Kawashima, “Development of a whole body training device by multi-directional force input using pneumatic artificial muscles,” 11th JFPS Int. Symp. on Fluid Power, GS3-03, 2021.
- [16] M. Yokota and M. Takaiwa, “Gait rehabilitation system using a non-wearing type pneumatic power assist device,” J. Robot. Mechatron., Vol.33, No.4, pp. 927-934, doi: 10.20965/jrm.2021.p0927, 2021.
- [17] J. C. Hong, H. Ohashi, and H. Iwata, “High-dorsiflexion assistive system for passive swing phase dorsiflexion training and preventing compensatory movements,” J. Robot. Mechatron., Vol.34, No.1, pp. 121-130, doi: 10.20965/jrm.2022.p0121, 2022.
- [18] N. Tsuda, T. Ehiro, Y. Nomura, and N. Kato, “Training to improve the landing of an uninjured leg in crutch walk using AR technology to present an obstacle,” J. Robot. Mechatron., Vol.33, No.5, pp. 1096-1103, doi: 10.20965/jrm.2021.p1096, 2021.
- [19] T. Togoe, P. H. Tung, K. Honda, Y. Nakashima, and M. Yamamoto, “Evaluation of muscle activity and human standing stability index using the swash plate in a disturbance application,” J. Robot. Mechatron., Vol.33, No.4, pp. 868-876, doi: 10.20965/jrm.2021.p0868, 2021.
- [20] S. M. O’Connor and A. D. Kuo, “Direction-dependent control of balance during walking and standing,” J. Neurophysiol, Vol.102, pp. 1411-1419, doi: 10.1152/jn.00131.2009, 2009.
- [21] M. W. Rogers and M. L. Mille, “Lateral stability and falls in older people,” Exercise and Sport Sciences Reviews, Vol.31, pp. 182-187, doi: 10.1097/00003677-200310000-00005, 2003.
- [22] C. W. Luchies, D. Wallace, R. Pazdur, S. Young, and A. J. DeYoung, “Effects of age on balance assessment using voluntary and involuntary step tasks,” J. of Grontology A Biological Sciences and Medical Sciences, Vol.54, No.3, pp. 140-144, doi: 10.1093/gerona/54.3.m140, 1999.
- [23] T. Arai, S. Obuchi, M. Kojima, S. Nishizawa, Y. Matsumoto, and Y. Inaba, “The relationship between age and change in physical functions after exercise intervention. Trainability of Japanese community-dwelling older elderly,” J. Jpn. Phys. Ther. Assoc., Vol.12, No.1, pp. 1-8, doi: 10.1298/jjpta.12.1,2009, 2009.
- [24] W. M. Paulus, A. Straube, and T. H. Brandt, “Visual stabilization of posture. Physiological stimulus characteristics and clinical aspects,” Brain, Vol.107, pp. 1143-1163, doi: 10.1093/brain/107.4.1143, 1984.
- [25] R. F. Raynolds and B. L. Day, “Fast visuomotor processing made faster by sound,” J. Physiology, Vol.583, pp. 1107-1115, doi: 10.1113/jphysiol.2007.136192, 2007.
- [26] P. C. Mahalanobis, “On the generalised distance in statistics,” Proc. of the National Institute of Science of India, Vol.2, pp. 49-55, 1936.
- [27] P. R. Cavanagh, “A technique for averaging center of pressure paths from a force platform,” J. Biomechanics, Vol.11, pp. 487-491, doi: 10.1016/0021-9290(78)90060-X, 1978.
- [28] A. L. Hof, M. G. Gazendam, and W. E. Sinke, “The condition for dynamic stability,” J. Biomech, Vol.38, pp. 1-8, doi: 10.1016/j.jbiomech.2004.03.025, 2005.
- [29] J. B. Geursen, D. Altena, C. H, Massen, and M. Verduin, “A model of the standing man for the description of his dynamic behavior,” Agressologie, Vol.18, pp. 63-69, 1976.
- [30] D. A. Winter, “Human balance and posture control during standing and walking,” Gait and Posture, Vol.3, pp. 193-214, doi: 10.1016/0966-6362(96)82849-9, 1995.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.