Paper:
Optimal Swing Support During Walking Using Wireless Pneumatic Artificial Muscle Driver
Haruki Toda*, Mitsunori Tada*, Tsubasa Maruyama*, and Yuichi Kurita**
*Artificial Intelligence Research Center, National Institute of Advanced Industrial Science and Technology (AIST)
2-3-26 Aomi, Koto-ku, Tokyo 135-0064, Japan
**Graduate School of Advanced Science and Engineering, Hiroshima University
1-3-2 Kagamiyama, Higashi-hiroshima City, Hiroshima 739-8511, Japan
This study evaluates the effect of swing support during walking using a wireless pneumatic artificial muscle (PAM) driver on hip and knee flexion angles. This driver can control two contraction parameters of the PAM: delay of contraction from the trigger and duration of contraction through a smartphone. Eleven healthy young individuals participated in this study. We asked the participants to walk with two PAMs attached to the left hip joint and a pressure sensor placed under the right heel to trigger the contraction. During the experiment, the contraction parameters were randomly changed: 0, 100, or 200 ms for the delay and 0, 100, 200, or 300 ms for the duration. The experimental results revealed significant differences in the hip and knee flexion angles, hip joint angular excursion, and stride length among the conditions. In addition, the optimal parameter differed among the subjects. It was confirmed that this individual variation was related to the walking speed of the subject, without PAM assistance.
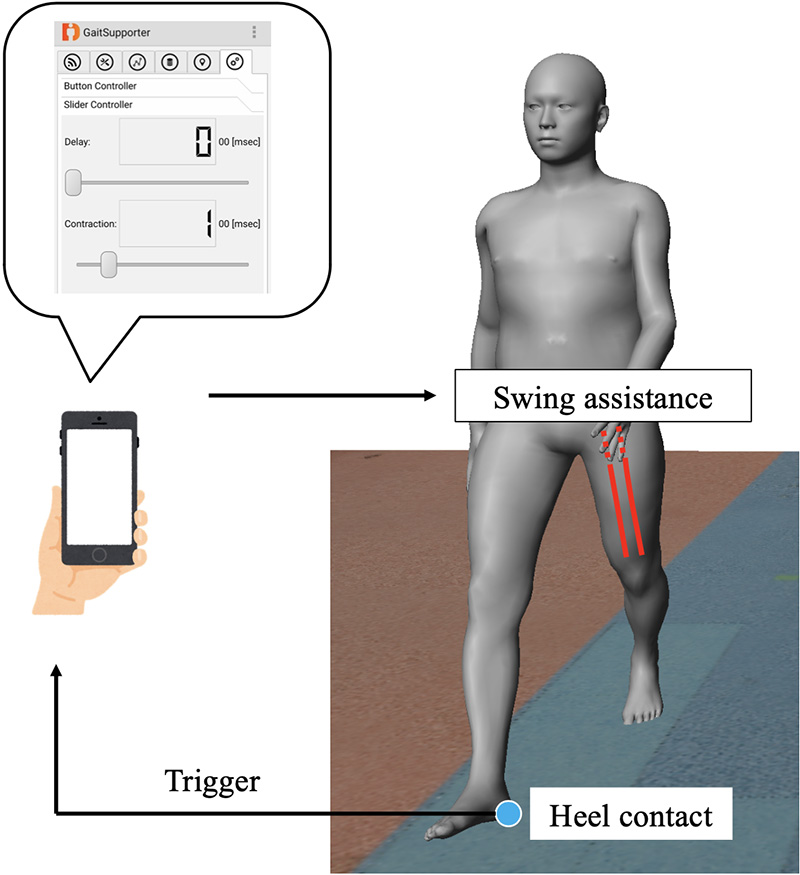
Schematic diagram of swing assistance
- [1] F. Pamoukdjian, E. Paillaud et al., “Measurement of gait speed in older adults to identify complications associated with frailty: A systematic review,” J. Geriatr. Oncol., Vol.6, No.6, pp. 484-496, 2015.
- [2] G. D. Caty, C. Arnould et al., “ABILOCO: A Rasch-Built 13-Item Questionnaire to Assess Locomotion Ability in Stroke Patients,” Arch. Phys. Med. Rehabil., Vol.89, No.2, pp. 284-290, 2008.
- [3] H. Shimada, H. Kim et al., “Factors Associated with the Timed Up and Go Test Score in Elderly Women,” J. Phys. Ther. Sci., Vol.22, No.3, pp. 273-278, 2010.
- [4] L. Z. Rubenstein, “Falls in older people: epidemiology, risk factors and strategies for prevention,” Age Ageing, Vol.35, No.suppl_2, pp. ii37-ii41, 2006.
- [5] M. P. Murray, A. B. Drought et al., “Walking patterns of normal men,” The J. of Bone and Joint Surgery, Vol.46, No.2, pp. 335-360, 1964.
- [6] S. J. Olney and C. Richards, “Hemiparetic gait following stroke. Part I: Characteristics,” Gait Posture, Vol.4, No.2, pp. 136-148, 1996.
- [7] R. G. Burdett, D. Borello-France et al., “Gait comparison of subjects with hemiplegia walking unbraced, with ankle-foot orthosis, and with Air-Stirrup® brace,” Phys. Ther., Vol.68, No.8, pp. 1197-1203, 1988.
- [8] K. Suzuki, G. Mito et al., “Intention-based walking support for paraplegia patients with Robot Suit HAL,” Advanced Robotics, Vol.21, No.12, pp. 1441-1469, 2007.
- [9] R. Riener, “Technology of the robotic gait orthosis Lokomat,” Springer, 2016.
- [10] M. F. Bruni, C. Melegari et al., “What does best evidence tell us about robotic gait rehabilitation in stroke patients: A systematic review and meta-analysis,” J. Clin. Neurosci., Vol.48, pp. 11-17, 2018.
- [11] T. Oba, H. Kadone et al., “Robotic Ankle–Foot Orthosis With a Variable Viscosity Link Using MR Fluid,” IEEE/ASME Trans. on Mechatronics, Vol.24, No.2, pp. 495-504, 2019.
- [12] C. Yokota, Y. Yamamoto et al., “Acute stroke rehabilitation for gait training with cyborg type robot Hybrid Assistive Limb: A pilot study,” J. Neurol. Sci., Vol.404, pp. 11-15, 2019.
- [13] K. Van Kammen, A. M. Boonstra et al., “Lokomat guided gait in hemiparetic stroke patients: the effects of training parameters on muscle activity and temporal symmetry,” Disabil. Rehabil., pp. 1-9, 2019.
- [14] L. Wallard, G. Dietrich et al., “Effects of robotic gait rehabilitation on biomechanical parameters in the chronic hemiplegic patients,” Neurophysiol. Clin., Vol.45, No.3, pp. 215-219, 2015.
- [15] P. Langhorne, J. Bernhardt et al., “Stroke rehabilitation,” The Lancet, Vol.377, No.9778, pp. 1693-1702, 2011.
- [16] C. Thakur, K. Ogawa et al., “Soft Wearable Augmented Walking Suit With Pneumatic Gel Muscles and Stance Phase Detection System to Assist Gait,” IEEE Robotics and Automation Letters, Vol.3, No.4, pp. 4257-4264, 2018.
- [17] J. C. Hong, S. Suzuki et al., “Development of high-dorsiflexion assistive robotic technology for gait rehabilitation,” 2018 IEEE Int. Conf. on Systems, Man, and Cybernetics (SMC), pp. 3801-3806, 2018.
- [18] Y. L. Park, B. R. Chen et al., “Design and control of a bio-inspired soft wearable robotic device for ankle-foot rehabilitation,” Bioinspiration and Biomimetics, Vol.9, No.1, 016007, 2014.
- [19] C. Thakur, K. Ogawa et al., “Active Passive Nature of Assistive Wearable Gait Augment Suit for Enhanced Mobility,” J. Robot. Mechatron., Vol.30, No.5, pp. 717-728, 2018.
- [20] T. Miyazaki, T. Tagami et al., “A Motion Control of Soft Gait Assistive Suit by Gait Phase Detection Using Pressure Information,” Applied Sciences, Vol.9, No.14, 2869, 2019.
- [21] H. Toda, M. Tada et al., “Effect of Contraction Parameters on Swing Support During Walking Using Wireless Pneumatic Artificial Muscle Driver: A Preliminary Study,” 2019 58th Annual Conf. of the Society of Instrument and Control Engineers of Japan (SICE), pp. 727-732, 2019.
- [22] M. Tada, “Wireless sensor and display modules for on-site motion measurement and intervention,” Proc. of the 19th System Integration Symp., pp. 418-422, 2019 (in Japanese).
- [23] T. Maruyama, M. Tada et al., “Constraint-Based Real-Time Full-Body Motion-Capture Using Inertial Measurement Units,” 2018 IEEE Int. Conf. on Systems, Man, and Cybernetics (SMC), pp. 4298-4303, 2018.
- [24] Y. Endo, M. Tada et al., “Dhaiba: development of virtual ergonomic assessment system with human models,” Proc. of the 3rd Int. Digital Human Symp., 2014.
- [25] M. A. Moosabhoy and S. A. Gard, “Methodology for determining the sensitivity of swing leg toe clearance and leg length to swing leg joint angles during gait,” Vol.24, No.4, pp. 493-501, 2006.
- [26] G. L. Smidt, “Hip Motion and Related Factors in Walking,” Phys. Ther., Vol.51, No.1, pp. 9-22, 1971.
- [27] P. M. Mills and R. S. Barrett, “Swing phase mechanics of healthy young and elderly men,” Human Movement Science, Vol.20, Nos.4-5, pp. 427-446, 2001.
- [28] C. Kirtley, M. W. Whittle et al., “Influence of walking speed on gait parameters,” J. Biomed. Eng., Vol.7, No.4, pp. 282-288, 1985.
- [29] F. Hebenstreit, A. Leibold et al., “Effect of walking speed on gait sub phase durations,” Human Movement Science, Vol.43, pp. 118-124, 2015.
- [30] I. A. K. de Quervain, S. R. Simon et al., “Gait pattern in the early recovery period after stroke,” The J. of Bone and Joint Surgery, Vol.78, No.10, pp. 1506-1514, 1996.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.