Paper:
Development and Evaluation of a Low Cost Cuffless Systolic Blood Pressure Device
Jörg Güttler, Muhammad Karim, Christos Georgoulas, and Thomas Bock
Chair of Building Realization and Robotics, Technische Universität München
Arcisstraße 21, 80333 München, Germany
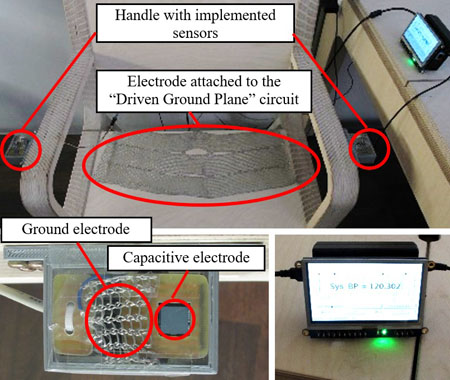
A cuffless blood pressure device implemented in a chair
- [1] D. J. Schofield, and J. R. Beard, “Baby boomer doctors and nurses: demographic change and transitions to retirement,” Medical J. of Australia, Vol.183, No.2, pp. 80-83, 2005.
- [2] J. K. Ninomiya, G. L’Italien, M. H. Criqui, J. L. Whyte, A. Gamst, and R. S. Chen, “Association of the Metabolic Syndrome With History of Myocardial Infarction and Stroke in the Third National Health and Nutrition Examination Survey,” Circulation, Vol.109, No.1, pp. 42-46, 2004.
- [3] P. Ernest, M. McCutcheon, F. Robert, and M. Rushmer, “Korotkoff Sounds An Experimental Critique,” Circulation Research, Vol.20, No.2, pp. 149-161, 1967.
- [4] U. Tholl, K. Frostner, and M. Anlauf, “Measuring blood pressure: pitfalls and recommendations,” Nephrology Dialysis Transplantation, Vol.19, No.4, pp. 766-770, 2004.
- [5] E. O’Brin, R. Asmar, L. Beilin, Y. Imai, J. Mallion, G. Mancia, T. Mengden, M. Myers, P. Paul, P. Palatini, G. Parati, T. Pickering, J. Redon, J. Staessen, G. Stergiou, and P. Verdecchia, “European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement,” J. of hypertension, Vol.21, No.5, pp. 821-848, 2003.
- [6] S. Leonhardt and A. Aleksandrowicz, “Non-Contact ECG Monitoring for Automotive Application,” Procs. of the 5th Inernational Workshop on Wearable and Implantable Body Sensor Networks, Hong Kong, 2008.
- [7] R. P. Smith, J. Argod, J.-L. Pépin, and P. A. Lévy, “Pulse transit time: an appraisal of potential clinical applications,” Thorax, Vol.54, No.5, pp. 452-457, 1999.
- [8] L. A. Geddes, M. H. Voelz, C. F. Babbs, J. D. Bourland, and W. A. Tacker, “Pulse transit time as an indicator of arterial blood pressure,” Psychophysiology, Vol.18, No.1, pp. 71-74, 1981.
- [9] P. Obrist, K. C. Light, J. A. McCubbin, J. Hutcheson, and J. L. Hoffer, “Pulse transit time: Relationship to blood pressure and myocardial performance,” Psychophysiology, Vol.16, No.3, pp. 292-301, 1979.
- [10] G. V. Marie, C. R. Lo, J. Van Jones, and D. W. Johnston, “The relationship between arterial blood pressure and pulse transit time during dynamic and static exercise,” Psychophysiology, Vol.21, No.5, pp. 521-527, 1984.
- [11] N. Yahagi and I. Yamada, “Relation Between Blood Pressure Estimated by Pulse Wave Velocity and Directly Measured Arterial Pressure,” J. of Robotics and Mechatronics, Vol.24, No.5, pp. 811-819, 2012.
- [12] J. Proença, J. Muehlsteff, X. Aubert, and P. Carvalho, “Is Pulse Transit Time a good indicator of Blood Pressure changes during short physical exercise in a young population?,” 32nd Annual Int. Conf. of the IEEE EMBS, Buenos Aires, Argentina, 2010.
- [13] H. Gesche, D. Grosskurth, G. Küchler, and A. Patzak, “Continuous blood pressure measurement by using the pulse transit time: comparison to a cuff-based method,” European J. of Applied Physiology, Vol.112, No.1, pp. 309-315, 2012.
- [14] J. Güttler, C. Georgoulas, T. Linner, and T. Bock, Evaluation of low cost capacitive ECG prototypes: A hardware/software approach, 17th Int. Conf. on Research and Education in Mechatronics (REM), 2016 11th France-Japan & 9th Europe-Asia Congress on Mechatronics (MECATRONICS), 2016.
- [15] H. Kemis, N. Bruce, W. Ping, T. Antonio, L. B. Gook, and H. J. Lee, “Healthcare Monitoring Application in Ubiquitous Sensor Network: Design and Implementation based on Pulse Sensor with Arduino,” 2012 6th Int. Conf. on New Trends in Information Science and Service Science and Data Mining (ISSDM), 2012.
- [16] Plessey semiconductors, “PS25203B EPIC Ultra High Impedance ECG Sensor Advance Information,” Data Sheet 291499 issue 3.
- [17] Plessey semiconductors, “PS25201B EPIC Ultra High Impedance ECG Sensor Advance Information.”
- [18] G. Coley, “BeagleBone Black System Reference Manual-Revision C.1,” 2014.
- [19] R. Betts and B. H. Brown, “Method for recording electrocardiograms with dry electrodes applied to unprepared skin,” Medical and biological engineering, Vol.14, No.3, pp. 313-315, 1976.
- [20] A. Aleksandrowicz, M. Walter, and S. Leonhard, “Ein kabelfreies, kapazitiv gekoppeltes EKG-Messsystem / Wireless ECG measurement system with capacitive coupling,” Biomedizinische Technik, Vol.52, No.2, pp. 185-192, 2007.
- [21] LOGIC supply, “XBEE CAPE MANUAL – BeagleBone Black XBee Prototyping Cape,” Revision 1.0, 2014.
- [22] S. Jain, A. Vaibhav, and L. Goyal, “Raspberry Pi based interactive home automation system through E-mail,” Int. Conf. on Optimization, Reliabilty, and Information Technology (ICROIT), 2014.
- [23] D. D. Bacquer, G. D. Backer, M. Kornitzer, and H. Blackburn, “Prognostic value of ECG findings for total, cardiovascular disease, and coronary heart disease death in men and women,” Heart, Vol.80, No.6, pp. 570-577, 1998.
- [24] J. Güttler, C. Georgoulas, and T. Bock, “Contactless Fever Measurement based on Thermal Imagery Analysis,” Sensors Applications Symposium (SAS), Catania, Italy, 2016.
- [25] Biocomfort Diagnostics GmbH, “tenso-comfort Blutdruckmessgerät BPM 105/BPM 205 Gebrauchsanweisung,” REF: 590007, 2006.
- [26] M. Middeke, “Arterielle Hypertonie Empfohlen von der Deutschen Hochdruckliga/Deutsche Hypertonie Gesellschaft,” Stuttgart: Georg Thieme Verlag KG, 2005.
- [27] P. Fung, G. Dumont, C. Ries, C. Mott and M. Ansermino, “Continuous Noninvasive Blood Pressure Measurement by Pulse Transit Time,” Procs. of the 26th Annual Int. Conf. of the IEEE EMBS, San Francisco, USA, 2004.
- [28] C. Poon and Y. Zhang, “Cuff-less and Noninvasive Measurements of Arterial Blood Pressure by Pulse Transit Time,” Engineering in Medicine and Biology 27th Annual Conf., Shanghai, China, 2005.
- [29] T. Bock, J. Güttler, C. Georgoulas, and T. Linner, “The Development of Intra-House Mobility, Logistics and Transfer Solutions in PASSAge,” J. of Robotics and Mechatronics, Vol.27, No.1, p. 108, 2015.
- [30] K. Toda, M. Fujioka, A. Fujii, S. Okawa, J. Shinohara, S. Tanaka, T. Nakamura, and T. Furuta, “A Home Healthcare System with Communication Robot Technologies – Development of Experimental Systems and in-Home Verification Experiments by Older Persons,” J. of Robotics and Mechatronics, Vol.23, No.6, pp. 951-968, 2011.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.