Paper:
Pneumatic Plantar Stimulation Device Replicating Manual Therapy Improves Lateral Stability in Standing Posture
Qi An*
 , Hiroyuki Hamada**
, Hiroyuki Hamada**
 , Shigeki Maruta***, Yuki Abe***, Kenichi Takada***, Ken Kikuchi*
, Shigeki Maruta***, Yuki Abe***, Kenichi Takada***, Ken Kikuchi*
 , Hiroshi Yamakawa**, Hajime Asama**
, Hiroshi Yamakawa**, Hajime Asama**
 , and Atsushi Yamashita*
, and Atsushi Yamashita*

*Department of Human and Engineered Environmental Studies, Graduate School of Frontier Sciences, The University of Tokyo
5-1-5 Kashiwanoha, Kashiwa, Chiba 227-8563, Japan
**Department of Precision Engineering, Graduate School of Engineering, The University of Tokyo
7-3-1 Hongo, Bunkyo, Tokyo 113-8656, Japan
***TechnoPro, Inc. TechnoPro Design Company
Roppongi Hills Mori Tower 35F, 6-10-1 Roppongi, Minato, Tokyo 106-6135, Japan
Strokes are a widespread condition characterized by motor paralysis and sensory impairment, and they significantly hinder daily activities. Hence, rehabilitation aimed at improving motor function is crucial for post-stroke patients. Manual therapy, which involves the manual stimulation of the limbs to provide sensory input and enhance motor function, is commonly employed for rehabilitation. However, the limited duration of inpatient rehabilitation highlights the need for devices that can provide similar rehabilitation interventions at home. Here we elucidate the skills employed by physical therapists during intervention through interviews and measurements of the force applied to the plantar surface of the foot. Subsequently, we develop a device capable of replicating these intervention skills. The investigation of physical-therapist skills revealed the importance of stimulating the muscles involved in forming the longitudinal and transverse arches and the flexor muscles of the toes during manual therapy. The required force for stimulation was also noted. Using our device, which utilized pneumatic actuation to replicate therapist skills, intervention on the plantar surface of the feet of healthy adults demonstrated improved stability in their standing posture, particularly in the lateral direction. These devices can enhance the sensory-motor connection from the plantar surface, thereby improving motor abilities, such as preventing falls.
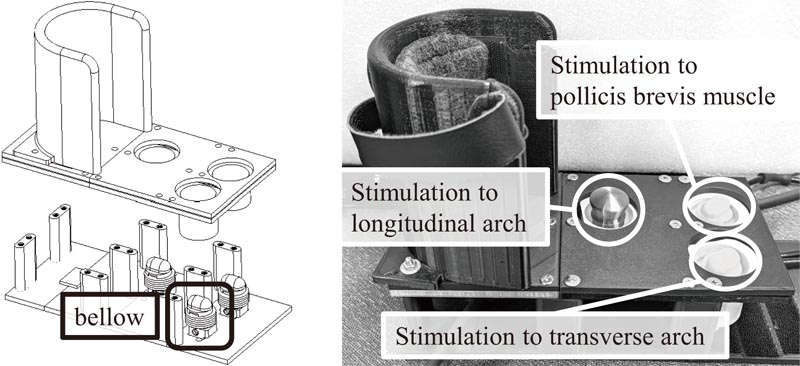
Plantar stimulation device replicating manual therapy
- [1] L. M. Carey, “Somatosensory loss after stroke,” Critical Reviews™ in Physical and Rehabilitation Medicine, Vol.7, Issue 1, pp. 51-91, 1995. https://doi.org/10.1615/CritRevPhysRehabilMed.v7.i1.40
- [2] S. F. Campfens, S. B. Zandvliet, C. G. Meskers, A. C. Schouten, M. J. van Putten, and H. van der Kooij, “Poor motor function is associated with reduced sensory processing after stroke,” Experimental Brain Research, Vol.233, pp. 1339-1349, 2015. https://doi.org/10.1007/s00221-015-4206-z
- [3] P. Kim, W. Sharon, M. Helen, and H. Margaret, “Quality of life of stroke survivors,” Quality of Life Research, Vol.8, No.4, pp. 293-301, 1999.
- [4] R. Yamamoto, S. Sasaki, W. Kuwahara, M. Kawakami, and F. Kaneko, “Effect of exoskeleton-assisted body weight-supported treadmill training on gait function for patients with chronic stroke: A scoping review,” J. of NeuroEngineering and Rehabilitation, Vol.19, Article No.143, 2022. https://doi.org/10.1186/s12984-022-01111-6
- [5] R. Kasai and S. Takeda, “The effect of a hybrid assistive limb® on sit-to-stand and standing patterns of stroke patients,” The J. of Physical Therapy Science, Vol.28, No.6, pp. 1786-1790, 2016. https://doi.org/10.1589/jpts.2016.1786
- [6] S. Shimooka, R. Suzuki, T. Uehara, T. Hirayama, and A. Gofuku, “Development of ankle-joint rehabilitation device for bedridden patient using fan-shaped pneumatic soft actuator driven at low pressure,” J. Robot. Mechatron., Vol.35, No.3, pp. 565-576, 2023. https://doi.org/10.20965/jrm.2023.p0565
- [7] C. J. Payne, E. G. Hevia, N. Phipps, A. Atalay, O. Atalay, B. Seo, D. J. Mooney, and C. J. Walsh, “Force Control of Textile-Based Soft Wearable Robots for Mechanotherapy,” Proc. of the 2018 IEEE Int. Conf. on Robotics and Automation (ICRA2018), pp. 5459-5465, 2018. https://doi.org/10.1109/ICRA.2018.8461059
- [8] S. J. Olney and C. Richards, “Hemiparetic gait following stroke. Part I: Characteristics,” Gait & Posture, Vol.4, Issue 2, pp. 136-148, 1996. https://doi.org/10.1016/0966-6362(96)01063-6
- [9] L. Bensoussan, S. Mesure, J.-M. Viton, and A. Delarque, “Kinematic and kinetic asymmetry in hemiplegic patients’ gait initiation patterns,” J. of Rehabilitation Medicine, Vol.38, No.2, pp. 287-294, 2006. https://doi.org/10.1080/16501970600694859
- [10] J. P. Regnaux, D. Pradon, N. Roche, J. Robertson, B. Bussel, and B. Dobkin, “Effects of loading the unaffected limb for one session of locomotor training on laboratory measures of gait in stroke,” Clinical Biomechanics, Vol.23, Issue 6, pp. 762-768, 2008. https://doi.org/10.1016/j.clinbiomech.2008.01.011
- [11] L. M. Carey and T. A. Matyas, “Training of somatosensory discrimination after stroke: facilitation of stimulus generalization,” American J. of Physical Medicine and Rehabilitation, Vol.84, No.6, pp. 428-442, 2005. https://doi.org/10.1097/01.phm.0000159971.12096.7f
- [12] P. O. McKeon, J. Hertel, D. Bramble, and I. Davis, “The foot core system: A new paradigm for understanding intrinsic foot muscle function,” British J. of Sports Medicine, Vol.49, No.290, pp. 1-9, 2015. https://doi.org/10.1136/bjsports-2014-094485
- [13] J. H. Hicks, “The mechanics of the foot. II. The plantar aponeurosis and the arch,” J. of Anatomy, Vol.88, No.1, pp. 25-30, 1954.
- [14] P. A. Tansey and P. J. Briggs, “Active and passive mechanisms in the control of heel supination,” Foot and Ankle Surgery, Vol.7, Issue 3, pp. 131-136, 2001. https://doi.org/10.1046/j.1460-9584.2001.00264.x
- [15] P. W. Lapidus, “Kinesiology and mechanical anatomy of the transverse tarsal joints,” Clinical Orthopaedics and Related Research, Vol.30, No.20, pp. 20-36, 1963.
- [16] K. A. Kirby, “Longitudinal arch load-sharing system of the foot,” Revista Española de Podología, Vol.28, pp. e18-e26, 2017.
- [17] R. M. Palmieri, C. D. Ingersoll, M. B. Stone, and B. A. Krause, “Center-of-pressure parameters used in the assessment of postural control,” J. of Sport Rehabilitation, Vol.11, No.1, pp. 51-66, 2002. https://doi.org/10.1123/jsr.11.1.51
- [18] S. Spry, C. Zebas, and M. Visser, “What is leg dominance?,” Proc. of the XI Symp. of the Int. Society of Biomechanics in Sports, pp. 165-168, 1993.
- [19] L. Aiello and C. Dean, “An introduction to human evolutionary anatomy,” Academic Press, 2002. https://doi.org/10.1016/C2009-0-02515-X
- [20] V. Weerdesteyn, M. de Niet, H. J. R. van Duijnhoven, and A. C. H. Geurts, “Falls in individuals with stroke,” J. of Rehabilitation Research and Development, Vol.45, No.8, pp. 1195-1213, 2008.
- [21] T. P. Knellwolf, A. R. Burton, E. Hammam, and E. V. G. Macefield, “Firing properties of muscle spindles supplying the intrinsic foot muscles of humans in unloaded and freestanding conditions,” J. of Neurophysiology, Vol.121, Issue 1, pp. 74-84, 2019. https://doi.org/10.1152/jn.00539.2018
- [22] D. J. Farris, L. A. Kelly, A. G. Cresswell, and G. A. Lichtwark, “The functional importance of human foot muscles for bipedal locomotion,” Proc. of National Academy of Sciences, Vol.116, No.5, pp. 1645-1650, 2019. https://doi.org/10.1073/pnas.1812820116
- [23] W. Wright, Y. Ivanenko, and V. Gurfinkel, “Foot anatomy specialization for postural sensation and control,” J. of Neurophysiology, Vol.107, Issue 5, pp. 1513-1521, 2012. https://doi.org/10.1152/jn.00256.2011
- [24] E. P. Mulligan and P. G. Cook, “Effect of plantar intrinsic muscle training on medial longitudinal arch morphology and dynamic function,” Manual Therapy, Vol.18, Issue 5, pp. 425-430, 2013. https://doi.org/10.1016/j.math.2013.02.007
- [25] D. S. Marigold and J. J. Eng, “The relationship of asymmetric weight-bearing with postural sway and visual reliance in stroke,” Gait & Posture, Vol.23, Issue 2, pp. 249-255, 2006.
- [26] M. Goliwas, P. Kocur, L. Furmaniuk, M. Majchrzycki, M. Wiernicka, and J. Lewandowski, “Effects of sensorimotor foot training on the symmetry of weight distribution on the lower extremities of patients in the chronic phase after stroke,” J. of Physical Therapy Science, Vol.27, pp. 2925-2930, 2015. https://doi.org/10.1589/jpts.27.2925
- [27] T. C. Christovão, H. Pasini, L. A. Grecco, L. A. Ferreira, N. A. Duarte, and C. S. Oliveira, “Effect of postural insoles on static and functional balance in children with cerebral palsy: A randomized controlled study,” Brazilian J. of Physical Therapy, Vol.19, Issue 1, pp. 44-51, 2015. https://doi.org/10.1590/bjpt-rbf.2014.0072
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.