Paper:
Development of a Spoon Motion Navigation Algorithm for the Mealtime Assistant Simulator
Atsushi Mitani* and Masumi Muramatsu**
*School of Design, Sapporo City University
1 Geijutsunomori, Minami-ku, Sapporo, Hokkaido 005-0864, Japan
**School of Nursing, Sapporo City University
Kita 11, Nishi 13, Chuo-ku, Sapporo, Hokkaido 060-0011, Japan
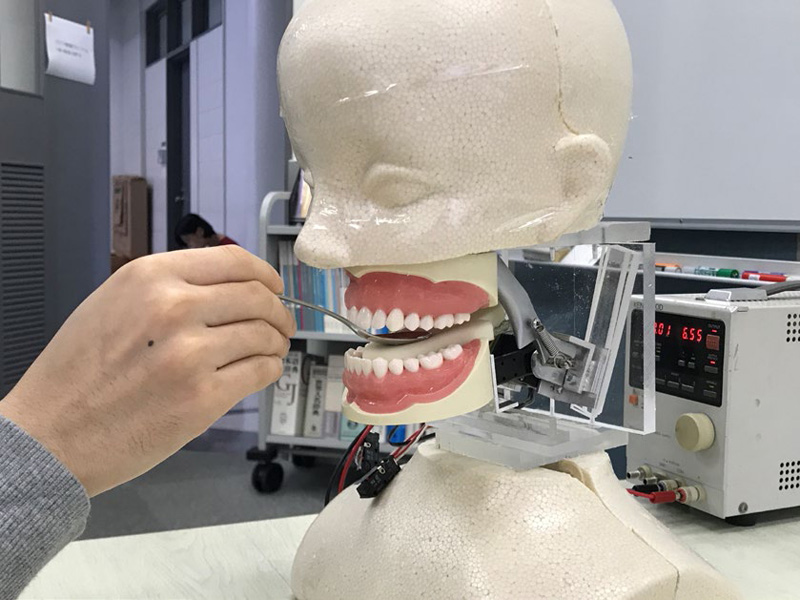
In aging society like Japan, maintaining the quality of life (QOL) is an important objective. The oral cavity has various significant functions that contribute to the QOL. Elderly people are susceptible to the swallowing disorders owing to various factors associated with advancing age. In such cases, mealtime assistance can provide elderly persons appropriate eating situations. Thus, mealtime assistance skills are essential for students in nursing and caregiver education. Recently, simulation education has attracted attention as an effective educational process for nursing and caregiver students before their clinical practice in a hospital or care house. In this educational process, a patient model that mimics specific symptoms called the simulation model, is used to learn the symptoms and its care process in the same clinical environment as actual. We have attempted to develop several oral care simulation models, and we have earlier developed a prototype of mealtime assistance simulation model. This simulation model had a tongue model with a sensor system to detect spoon motions, and its fundamental functions were evaluated via spoon detection experiments. Based on the earlier achievements, in this study, we develop an evaluation system of feeding skill using a spoon. The pressing force and position by spoon on the tongue model were estimated by transfer functions derived from experiments. In addition, we developed an algorithm that leads students’ spoon position and pressing force in the correct position.
Mealtime assistant simulator
- [1] The Ministry of Health, Labour and Welfare Japan, “The report of review meeting on contents and method of nursing education,” February 28, 2011 (in Japanese).
- [2] T. Daigo, M. Muramatsu, and A. Mitani, “Development of the Second Prototype of an Oral Care Simulator,” J. Robot. Mechatron., Vol.33, No.1, pp. 172-179, 2021.
- [3] A. Mitani and M. Muramatsu, “Development of Human Tongue Model for Mealtime Assistant Training Using Oral Care Simulation Model,” Int. J. Automation Technol., Vol.13, No.4, pp. 499-505, 2019.
- [4] T. Hashimoto, Y. Takakura, T. Hamada, T. Akazawa, and M. Yamamoto, “Development of Foot Gait Simulator for Presenting Environment to Each User,” J. Adv. Comput. Intell. Intell. Inform., Vol.15, No.5, pp. 554-562, 2011.
- [5] K. Tokoro, T. Hashimoto, and H. Kobayashi, “Development of Robotic Defecation Simulator,” J. Robot. Mechatron., Vol.26, No.3, pp. 377-387, 2014.
- [6] Y. Takahashi and T. Yatsumonji, “Going out experience robot for bedridden people by remote control system,” Proc. of 39th SICE Annual Conf., Int. Session Papers (IEEE Cat. No.00TH8545), pp. 175-178, 2000.
- [7] Y.-Y. Jiang and W.-T. Hu, “The Study of Practical Teaching of Oral Health Education Named “Going-Out”,” Proc. of 7th Int. Conf. on Information Technology in Medicine and Education (ITME), pp. 13-15, 2015.
- [8] S. Changping, “Application of SimMan universal patient simulator in the teaching of medical nursing,” Proc. of 2011 Int. Conf. on Human Health and Biomedical Engineering, pp. 1172-1174, 2011.
- [9] T. Torregrosa et al., “Fabrication of a nursing manikin overlay for simulation of chest drainage management,” Proc. of 2015 IEEE Great Lakes Biomedical Conference (GLBC), pp. 1-4, 2015.
- [10] P. Clavario et al., “Use of an arrhythmia simulator for the evaluation of nurses’ knowledge and as a teaching tool,” Proc. of 1995 Computers in Cardiology, pp. 621-624, 1995.
- [11] X.-L. Lu, “System design and development for a CSCW based remote oral medical diagnosis system,” Proc. of 2005 Int. Conf. on Machine Learning and Cybernetics, Vol.6, pp. 3698-3703, 2005.
- [12] C.-J. Hou et al., “Computer-aided auscultation learning system for nursing technique instruction,” Proc. of 30th Annual Int. Conf. of the IEEE Engineering in Medicine and Biology Society, pp. 1575-1578, 2008.
- [13] G. J. Gerling et al., “The Design and Evaluation of a Computerized and Physical Simulator for Training Clinical Prostate Exams,” IEEE Trans. on Systems, Man, and Cybernetics – Part A: Systems and Humans, Vol.39, No.2, pp. 388-403, 2009.
- [14] L. Mudura et al., “A Virtual Nursing Simulator with Haptic Feedback for Nasotracheal Suctioning,” Proc. of 2006 IEEE/RSJ Int. Conf. on Intelligent Robots and Systems, pp. 698-703, 2006.
- [15] M. Chiba and K. Hamamoto, “Development of Learning Support System on Auscultation for Nurse Using Virtual Reality,” Proc. of 2018 2nd Int. Conf. on Biomedical Engineering (IBIOMED), pp. 34-38, 2018.
- [16] H. Takanobu et al., “Dental Patient Robot as a Mechanical Human Simulator,” Proc. of 2007 IEEE Int. Conf. on Mechatronics, pp. 1-6, doi: 10.1109/ICMECH.2007.4280065, 2007.
- [17] Y. Aoki, S. Kabuto, Y. Ozeki, T. Tanaka, and K. Ota, “The effect of tongue pressure strengthening exercise for dysphagic patients,” Japanese J. of Comprehensive Rehabilitation Science, No.6, pp. 129-136, 2015.
- [18] Y. Utanohara et al., “Standard values of maximum tongue pressure taken using newly developed disposable tongue pressure measurement device,” Dysphagia, Vol.23, No.3, Article 286, doi: 10.1007/s00455-007-9142-z, 2008.
- [19] T. Nantoi et al., “Development of a new tongue-palate contact training with a spring scale,” Japanese J. of Speech, Language, and Hearing Research, Vol.15, No.2, pp. 62-70, 2018 (in Japanese).
- [20] M. G. M. H. Florie, W. Pilz et al., “The Effect of Cranial Nerve Stimulation on Swallowing: A Systematic Review,” Dysphagia, Vol.36, pp. 216-230, doi: 10.1007/s00455-020-10126-x, 2021.
- [21] Y. Tanaka, “Spoon technic to extract oral function,” Dementia Care Cases J., Vol.8, No.2, pp. 135-143, 2015 (in Japanese).
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.