Paper:
Evaluating the Effectiveness of a Vascular Access Imaging Device Used in Training Recently Graduated Nurses
Yutaka Murakami*, Yuko Ohno**, Miki Nishimura**, Michiko Kido**, and Kenji Yamada**
*Kobe Adventist Hospital
8-4-1 Arinodai, Kita-ku, Kobe, Hyogo 651-1321, Japan
**Osaka University
2-2 Yamadaoka, Suita, Osaka 565-0871, Japan
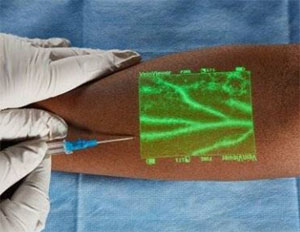
The VAID helps to select proper IV insertion sites
- [1] M. Kaur and S. Kaur, “Methods to increase peripheral veins visualization in patients getting chemotherapy,” Int. J. of Nursing Education, Vol.4, pp. 1-3, 2012.
- [2] S. F. Smith, D. J. Duell, and B. C. Martin, “Clinical Nursing Skills: Basic to Advanced Skills (7th Edition),” Stanford, Ct: Appleton & Lange, 2007.
- [3] M. Yokota and R. Kawashima, “Circumstances and Problems for Practice of Intravenous Injections by Nurses,” Bulletin of Fukushima School of Nursing, Vol.11, pp. 39-48, 2009 (in Japanese).
- [4] A. F. Jacobson and E. H. Winslow, “Variables influencing intravenous catheter insertion difficulty and failure: An analysis of 339 intravenous catheter insertion,” Heart & Lung, Vol.34, No.5, pp. 345-359, 2005.
- [5] A. E. Bair, J. S. Rose, C. W. Vance, E. Andrada-Brown, and N. Kuppermann, “Ultrasound-assisted peripheral venous access in young children: a randomized controlled trial and pilot feasibility study,” The Western J. of Emergency Medicine, Vol.9, pp. 219-224, 2008.
- [6] K. A. Peterson, A. L. Phillips, E. Truemper, and S. Agrawal, “Does the Use of an Assistive Device by Nurses Impact Peripheral Intravenous Catheter Insertion Success in Children?,” J. of Pediatric Nursing, Vol.27, pp. 134-143, 2012.
- [7] M. C. K. Do Amaral and M. A. M. Pettengill, “Using ultrasound to guide peripheral venipuncture in children: The importance of the technique for nurses,” ACTA Paulista de Enfermagem, Vol.23, pp. 472-478, 2010.
- [8] T. Reeves and D. Morrison, “An Innovative Nurse-Driven Ultrasound-Guided Peripheral IV Program for Medical Surgical and Progressive Care Units: From Concept to Implementation,” J. of the Association for Vascular Access, Vol.18, pp. 213-213, 2013.
- [9] M. D. Witting, S. M. Schenkel, B. J. Lawner, and B. D. Euerle, “Ultrasound in emergency medicine: Effects of Vein Width and Depth on Ultrasound-Guided Peripheral Intravenous Success Rates,” J. of Emergency Medicine, Vol.39, pp. 70-75, 2010.
- [10] C.-Y. Sun, K.-C. Lee, I.-H. Lin, C.-L. Wu, H.-P. Huang, Y.-Y. Lin, Y.-F. Hsu, and H.-R. Yu, “Original article: Near-infrared Light Device Can Improve Intravenous Cannulation in Critically Ill Children,” Pediatrics & Neonatology, Vol.54, pp. 194-197, 2013.
- [11] M. Kim, J. Park, N. Rhee, S. Je, S. Hong, Y. Lee et al, “Efficacy of VeinViewer in pediatric peripheral intravenous access: a randomized controlled trial,” European J. of Pediatrics, Vol.171, p. 1121, July 2012.
- [12] N. J. Cuper, J. H. Klaessens, J. E. Jaspers, R. de Roode, H. J. Noordmans, J. C. de Graaff, and R. M. Verdaasdonk, “The use of near-infrared light for safe and effective visualization of subsurface blood vessels to facilitate blood withdrawal in children,” Medical Engineering and Physics, Vol.35, pp. 433-440, 2013.
- [13] J. C. de Graaff, N. J. Cuper, R. A. A. Mungra, K. Vlaardingerbroek, S. C. Numan and C. J. Kalkman, “Near-infrared light to aid peripheral intravenous cannulation in children: a cluster randomized clinical trial of three devices,” Anesthesia, Vol.68, pp. 835-845, 2013.
- [14] D. J. L.-M. Wiegand and N. American Association of Critical-Care, “AACN Procedure Manual for Critical Care,” St. Louis, Mo: Elsevier/Saunders, 2011.
- [15] S. J. Brown, “Knowledge For Health Care Practice: A Guide to Using Research evidence,” Philadelphia, Pa: W. B. Saunders Company, 1999.
- [16] M. B. F. Makic, S. A. Martin, S. Burns, D. Philbrick, and C. Rauen, “Putting Evidence Into Nursing Practice: Four Traditional Practices Not Supported by the Evidence,” Critical Care Nursing, Vol.33, pp. 28-42, 2013.
- [17] Griffis University, “Peripheral Intravenous Access and Care,” Course syllabus, 2010.
- [18] F. Y. Tee, C. S. L. Low, and P. Matizha, “Patient Perceptions and Experience of Pain, Anxiety and Comfort during Peripheral Intravenous Cannulation in Medical Wards: Topical Anesthesia, Effective Communication, and Empowerment,” Int. J. of Nursing Science, Vol.5, pp. 41-46, 2015.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.