Letter:
Urinary Sodium/Potassium Ratio Index Estimates Ionic Balance in Humans
Yutaka Yoshida
 , Yuta Tarusawa, Asahi Nishimura, and Emi Yuda†
, Yuta Tarusawa, Asahi Nishimura, and Emi Yuda†

Graduate School of Information Sciences, Tohoku University
6-3-09 Aza-Aoba, Aramaki, Aoba-ku, Sendai, Miyagi 980-8579, Japan
†Corresponding author
This study measured the urinary sodium/potassium (U-Na/K) ratio using a compact ion meter to verify whether the U-Na/K ratio can estimate human blood pressure (BP) and ionic balance. The U-Na/K ratio and BP were measured in five healthy participants (including one female) after urination for at least two days per person, and lifestyle information, such as exercise and diet, were recorded at the time of measurement. Analysis of the measured data at 57 points revealed no significant difference in the U-Na/K ratio and BP, but a significant decrease in the U-Na/K ratio was observed after exercise accompanied by sweating (P = 0.01). Although previous studies have demonstrated that sodium is released by sweating, its measurement is difficult. Measuring sodium/potassium ratio is useful for preventing heatstroke and may serve as an explanatory variable for sweating and exercise intensity.
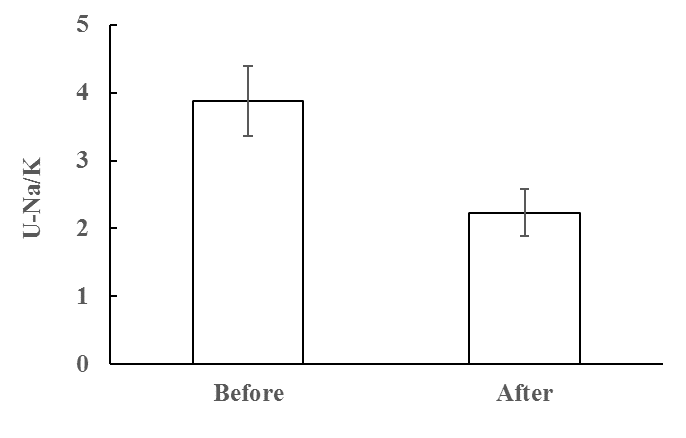
U-Na/K of before and after workout.
- [1] Y. Ma et al., “24-hour urinary sodium and potassium excretion and cardiovascular risk,” N. Engl. J. Med., Vol.386, No.3, pp. 252-263, 2022. https://doi.org/10.1056/NEJMoa2109794
- [2] V. Perez and E. T. Chang, “Sodium-to-potassium ratio and blood pressure, hypertension, and related factors,” Adv. Nutr., Vol.5, No.6, pp. 712-741, 2014. https://doi.org/10.3945/an.114.006783
- [3] H. J. Adrogué and N. E. Madias, “The impact of sodium and potassium on hypertension risk,” Semin. Nephrol., Vol.34, No.3, pp. 257-272, 2014. https://doi.org/10.1016/j.semnephrol.2014.04.003
- [4] A. Binia et al., “Daily potassium intake and sodium-to-potassium ratio in the reduction of blood pressure: A meta-analysis of randomized controlled trials,” J. Hypertens., Vol.33, No.8, pp. 1509-1520, 2015. https://doi.org/10.1097/HJH.0000000000000611
- [5] H. J. Yang et al., “Associations between metabolic syndrome and urinary Na-to-K ratio and glomerular filtration rate in middle-aged adults regardless of Na and K intakes,” Clin. Exp. Nephrol., Vol.24, No.11, pp. 1015-1024, 2020. https://doi.org/10.1007/s10157-020-01933-5
- [6] S. S. Hedayati et al., “Association of urinary sodium/potassium ratio with blood pressure: Sex and racial differences,” Clin. J. Am. Soc. Nephrol., Vol.7, No.2, pp. 315-322, 2012. https://doi.org/10.2215/CJN.02060311
- [7] P. Rust and C. Ekmekcioglu, “Impact of salt intake on the pathogenesis and treatment of hypertension,” M. S. Islam (Ed.), “Hypertension: From Basic Research to Clinical Practice, Vol. 2,” pp. 61-84, Springer, 2017. https://doi.org/10.1007/5584_2016_147
- [8] J. Chmielewski and J. B. Carmody, “Dietary sodium, dietary potassium, and systolic blood pressure in US adolescents,” J. Clin. Hypertens., Vol.19, No.9, pp. 904-909, 2017. https://doi.org/10.1111/jch.13014
- [9] F. C. Luft, N. S. Fineberg, and R. N. Sloan, “Overnight urine collection to estimate sodium intake,” Hypertension, Vol.4, No.4, pp. 494-498, 1982. https://doi.org/10.1161/01.HYP.4.4.494
- [10] J. T. Knuiman et al., “Multiple overnight urine collections may be used for estimating the excretion of electrolytes and creatinine,” Clin. Chem., Vol.34, No.1, pp. 135-138, 1988. https://doi.org/10.1093/clinchem/34.1.135
- [11] J. He et al., “Agreement between overnight and 24-hour urinary cation excretions in Sourthern Chinese men,” Am. J. Epidemiol., Vol.137, No.11, pp. 1212-1220, 1993. https://doi.org/10.1093/oxfordjournals.aje.a116623
- [12] J. Staessen et al., “The assessment of the relationship between blood pressure and sodium intake using whole-day, daytime and overnight urine collections,” J. Hypertens., Vol.9, No.11, pp. 1035-1040, 1991. https://doi.org/10.1097/00004872-199111000-00009
- [13] K. Yamasue et al., “Methods for self-monitoring of daily salt and potassium intake at home,” Jpn. J. Cardiovasc. Dis. Prev., Vol.39, No.3, pp. 157-163, 2004 (in Japanese). https://doi.org/10.11381/jjcdp2001.39.157
- [14] OMRON, HEU-001F Na+K+scan (in Japanese). https://www.healthcare.omron.co.jp/medical/products/HEU-001F/index.html [Accessed August 1, 2022]
- [15] H. Nose, Y. Kamijo, and S. Masuki, “Interactions between body fluid homeostasis and thermoregulation in humans,” Handb. Clin. Neurol., Vol.156, pp. 417-429, 2018. https://doi.org/10.1016/b978-0-444-63912-7.00025-4
- [16] H. Onda and H. Yokota, “Risk factors of heatstroke,” Jpn. J. Clin. Med., Vol.70, No.6, pp. 947-951, 2012 (in Japanese).
- [17] R. J. Maughan, J. B. Leiper, and S. M. Shirreffs, “Restoration of fluid balance after exercise-induced dehydration: Effects of food and fluid intake,” Eur. J. Appl. Physiol. Occup. Physiol., Vol.73, Nos.3-4, pp. 317-325, 1996. https://doi.org/10.1007/bf02425493
- [18] J. P. Mallié et al., “Renal handling of salt and water in humans during exercise with or without hydration,” Eur. J. Appl. Physiol., Vol.86, No.3, pp. 196-202, 2002. https://doi.org/10.1007/s00421-001-0524-x
- [19] R. J. Maughan et al., “Post-exercise rehydration in man: Effects of electrolyte addition to ingested fluids,” Eur. J. Appl. Physiol. Occup. Physiol., Vol.69, No.3, pp. 209-215, 1994. https://doi.org/10.1007/bf01094790
- [20] F. Brouns, E. M. Kovacs, and J. M. Senden, “The effect of different rehydration drinks on post-exercise electrolyte excretion in trained athletes,” Int. J. Sports Med., Vol.19, No.1, pp. 56-60, 1998. https://doi.org/10.1055/s-2007-971881
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.