Paper:
Evaluation of Frailty and Fall Risk Using Acceleration in a Low-Physical-Strain Five Times Sit-to-Stand Test
Takumi Nunokawa*,†, Minoru Morita*
 , Keiko Doi**
, Keiko Doi**
 , Tsunahiko Hirano**
, Tsunahiko Hirano**
 , Kazuto Matsunaga**, and Zhongwei Jiang*
, Kazuto Matsunaga**, and Zhongwei Jiang*
*Graduate School of Sciences and Technology for Innovation, Yamaguchi University
2-16-1 Tokiwadai, Ube, Yamaguchi 755-8611, Japan
†Corresponding author
**Graduate School of Medicine, Yamaguchi University
1-1-1 Minami-kogushi, Ube, Yamaguchi 755-8505, Japan
Early detection of frailty is crucial for older adults’ health, particularly as lower limb muscle strength declines rapidly in the early stages of frailty. The five times sit-to-stand (FTSTS) test is commonly used to evaluate this strength. However, performing the FTSTS test at maximum effort poses risks, requiring assistance to prevent falls and increasing the likelihood of excessive strain on lower limb joints. Therefore, safer, less strenuous methods for assessing muscle strength are needed to minimize these risks. Therefore, to measure lower limb function in a safe environment, it is necessary to implement a version of the FTSTS test that does not require maximum effort speed, allowing the subject to perform at their own pace with minimal physical strain, and to develop a method to automate this measurement. This study proposes a method to assess frailty and fall risk by conducting the FTSTS test with minimal exertion and analyzing acceleration data. A system using a wearable accelerometer with wireless communication capabilities was developed to automatically measure the acceleration during the sit-to-stand movements. The J-CHS (Japanese version of the Cardiovascular Health Study) criteria for frailty diagnosis and the Kihon Checklist for fall risk assessment were conducted, and the results were used as a control for categorizing subjects based on frailty and fall risk. Clinical trials of the FTSTS test were conducted on older adults, and frailty and fall risk were assessed based on the acceleration data obtained to verify the effectiveness of the proposed method.
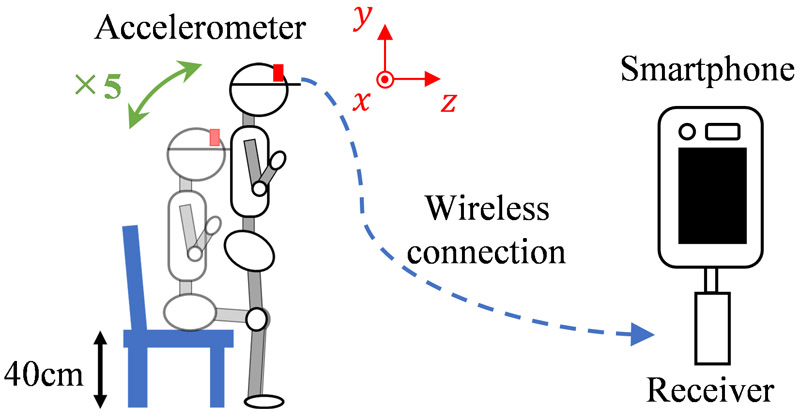
Overview of the FTSTS test conducted in this study
- [1] K. Kin, K. Kushida, K. Yamazaki, S. Okamoto, and T. Inoue, “Bone mineral density of the spine in normal Japanese subjects using dual-energy X-ray absorptiometry: Effect of obesity and menopausal status,” Calcif. Tissue Int., Vol.49, No.2, pp. 101-106, 1991. https://doi.org/10.1007/BF02565129
- [2] J. Lexell, C. C. Taylor, and M. Sjöström, “What is the cause of the ageing atrophy?: Total number, size and proportion of different fiber types studied in whole vastus lateralis muscle from 15- to 83-year-old men,” J. Neurol. Sci., Vol.84, No.2, pp. 275-294, 1988. https://doi.org/10.1016/0022-510X(88)90132-3
- [3] S. Muraki et al., “Prevalence of radiographic knee osteoarthritis and its association with knee pain in the elderly of Japanese population-based cohorts: The ROAD study,” Osteoarthr. Cartil., Vol.17, No.9, pp. 1137-1143, 2009. https://doi.org/10.1016/j.joca.2009.04.005
- [4] K. Nakamura, “A ‘super-aged’ society and the ‘locomotive syndrome’,” J. Orthop. Sci., Vol.13, No.1, pp. 1-2, 2008. https://doi.org/10.1007/s00776-007-1202-6
- [5] A. Clegg, J. Young, S. Iliffe, M. O. Rikkert, and K. Rockwood, “Frailty in elderly people,” Lancet, Vol.381, No.9868, pp. 752-762, 2013. https://doi.org/10.1016/S0140-6736(12)62167-9
- [6] I. Janssen, S. B. Heymsfield, Z. Wang, and R. Ross, “Skeletal muscle mass and distribution in 468 men and women aged 18–88 yr,” J. Appl. Physiol., Vol.89, No.1, pp. 81-88, 2000. https://doi.org/10.1152/jappl.2000.89.1.81
- [7] Q.-L. Xue, K. Bandeen-Roche, R. Varadhan, J. Zhou, and L. P. Fried, “Initial manifestations of frailty criteria and the development of frailty phenotype in the women’s health and aging study II,” J. Gerontol.: Ser. A, Vol.63, No.9, pp. 984-990, 2008. https://doi.org/10.1093/gerona/63.9.984
- [8] S. R. Lord, S. M. Murray, K. Chapman, B. Munro, and A. Tiedemann, “Sit-to-stand performance depends on sensation, speed, balance, and psychological status in addition to strength in older people,” J. Gerontol.: Ser. A, Vol.57, No.8, pp. M539-M543, 2002. https://doi.org/10.1093/gerona/57.8.M539
- [9] R. W. Bohannon, “Reference values for the five-repetition sit-to-stand test: A descriptive meta-analysis of data from elders,” Percept. Mot. Ski., Vol.103, No.1, pp. 215-222, 2006. https://doi.org/10.2466/pms.103.1.215-222
- [10] S. Buatois et al., “A simple clinical scale to stratify risk of recurrent falls in community-dwelling adults aged 65 years and older,” Phys. Ther., Vol.90, No.4, pp. 550-560, 2010. https://doi.org/10.2522/ptj.20090158
- [11] J. M. Guralnik, L. Ferrucci, E. M. Simonsick, M. E. Salive, and R. B. Wallace, “Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability,” N. Engl. J. Med., Vol.332, No.9, pp. 556-562, 1995. https://doi.org/10.1056/NEJM199503023320902
- [12] K. E. Ensrud et al., “Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women,” Arch. Intern. Med., Vol.168, No.4, pp. 382-389, 2008. https://doi.org/10.1001/archinternmed.2007.113
- [13] W. Zijlstra, R. W. Bisseling, S. Schlumbohm, and H. Baldus, “A body-fixed-sensor-based analysis of power during sit-to-stand movements,” Gait Posture, Vol.31, No.2, pp. 272-278, 2010. https://doi.org/10.1016/j.gaitpost.2009.11.003
- [14] G. Bochicchio et al., “Temporal, kinematic and kinetic variables derived from a wearable 3D inertial sensor to estimate muscle power during the 5 sit to stand test in older individuals: A validation study,” Sensors, Vol.23, No.10, Article No.4802, 2023. https://doi.org/10.3390/s23104802
- [15] G. R. H. Regterschot, W. Zhang, H. Baldus, M. Stevens, and W. Zijlstra, “Accuracy and concurrent validity of a sensor-based analysis of sit-to-stand movements in older adults,” Gait Posture, Vol.45, pp. 198-203, 2016. https://doi.org/10.1016/j.gaitpost.2016.02.004
- [16] S. Satake et al., “Prevalence of frailty among community-dwellers and outpatients in Japan as defined by the Japanese version of the Cardiovascular Health Study criteria,” Geriatr. Gerontol. Int., Vol.17, No.12, pp. 2629-2634, 2017. https://doi.org/10.1111/ggi.13129
- [17] S. Satake, K. Kinoshita, Y. Matsui, and H. Arai, “Physical domain of the Kihon Checklist: A possible surrogate for physical function tests,” Geriatr. Gerontol. Int., Vol.20, No.6, pp. 644-646, 2020. https://doi.org/10.1111/ggi.13916
- [18] L. P. Fried et al., “Frailty in older adults: Evidence for a phenotype,” J. Gerontol.: Ser. A, Vol.56, No.3, pp. M146-M157, 2001. https://doi.org/10.1093/gerona/56.3.M146
- [19] S. Satake et al., “Validity of the Kihon Checklist for assessing frailty status,” Geriatr. Gerontol. Int., Vol.16, No.6, pp. 709-715, 2016. https://doi.org/10.1111/ggi.12543
- [20] K. Tateoka, T. Tsuji, T. Shoji, S. Tokunaga, and T. Okura, “Relationship between acceleration in a sit-to-stand movement and physical function in older adults,” Geriatrics, Vol.8, No.6, Article No.123, 2023. https://doi.org/10.3390/geriatrics8060123
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.