Paper:
Electrical Muscle Stimulation to Develop and Implement Menstrual Simulator System
Chihiro Asada*1, Kotori Tsutsumi*1, Yuichi Tamura*2, Naoya Hara*3, Wataru Omori*4, Yuta Otsuka*5, and Katsunari Sato*1
*1Nara Women’s University
Kitauoyanishimachi, Nara 630-8506, Japan
*2Konan University
8-9-1 Okamoto, Higashinada-ku, Kobe, Hyogo 658-8501, Japan
*3Osaka University
1-1 Yamadaoka, Suita, Osaka 658-8501, Japan
*4Japan Advanced Institute of Science and Technology
1-1 Asahidai, Nomi, Ishikawa 923-1292, Japan
*5University of Hyogo
7-1-28 Minatojimaminamimachi, Chuo-ku, Kobe, Hyogo 650-0047, Japan
Menstrual symptoms and cycles are complex, and the associated discomfort is difficult to quantify. Therefore, men, and some women, do not completely understand them. Here, we propose a system that simulates menstruation-like cramps through electrical muscle stimulation (EMS). We conducted an experiment to compare and evaluate the natural and electrically stimulated menstrual cramps. The results show that menstrual cramps using EMS can reproduce the nature of periodic dull pain. However, in this study, the position where the pain occurred was shallow. Furthermore, we constructed a demonstration system based on the proposed method. From the exhibition, we confirmed that this experience can help verbalize menstrual-related discomfort and allow people to better understand menstrual symptoms. In other words, this experience will help eliminate negative perception of menstruation.
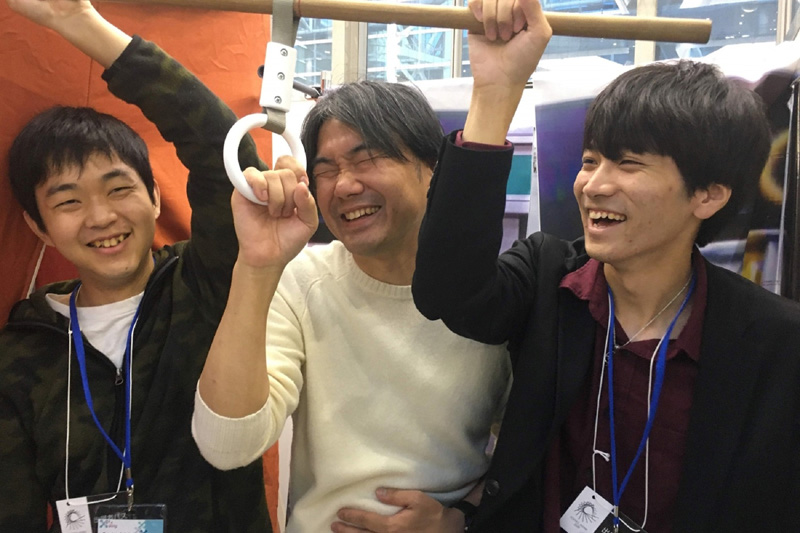
Actual experience in exhibition
- [1] M. E. Schoep, T. E. Nieboer, M. van der Zanden, D. D. M. Braat, and A. W. Nap, “The impact of menstrual symptoms on everyday life: a survey among 42,879 women,” American J. of Obstetrics and Gynecology, Vol.220, Issue 6, pp. 569.e1-569.e7, 2019.
- [2] I. S. Fraster, H. O. Critchley, M. Broder, and M. G. Munro, “The FIGO recommendations on terminologies and definitions for normal and abnormal uterine bleeding,” Seminars in reproductive medicine, Vol.29, No.5, pp. 383-390, 2011.
- [3] M. Krijn, P. M. G. Emmelkamp, R. P. Olafsson, and R. Biemond, “Virtual reality exposure therapy of anxiety disorders: A review,” Clinical Psychology Review, Vol.24, Issue 3, pp. 259-281, 2004.
- [4] D. A. Das, K. A. Grimmer, A. L. Sparnon, S. E. McRae, and B. H. Thomas, “The efficacy of playing a virtual reality game in modulating pain for children with acute burn injuries: a randomized controlled trial [ISRCTN87413556],” BMC Pediatrics, Vol.5, pp. 1-10, 2005.
- [5] S. M. Schneider and M. L. Workman, “Virtual reality as a distraction intervention for older children receiving chemotherapy,” Pediatric Nursing, Vol.26, No.6, p. 593, 2000.
- [6] J. Gershon, E. Zimand, M. Pickering, B. O. Rothbaum, and L. Hodges, “A pilot and feasibility study of virtual reality as a distraction for children with cancer,” J. of the American Academy of Child & Adolescent Psychiatry, Vol.43, Issue 10, pp. 1243-1249, 2004.
- [7] B. Garrett, T. Taverner, D. Gromala, G. Tao, E. Cordingley, and C. Sun, “Virtual Reality Clinical Research: Promises and Challenges,” JMIR Serious Games, Vol.6, Issue 4, e10839, 2018.
- [8] L. Li, F. Yu, D. Shi, J. Shi, Z. Tian, J. Yang, and Q. Jiang, “Application of virtual reality technology in clinical medicine,” American J. of translational research, Vol.9, Issue 9, pp. 3867-3880, 2017.
- [9] M. M. Tse, J. K. Ng, J. W. Chung, and T. K. Wong, “The application of eyeglass displays in changing the perception of pain,” Studies in Health Technology and Informatics, Vol.85, pp. 532-535, 2002.
- [10] F. Magora, S. Cohen, M. Shochina, and E. Dayan, “Virtual reality immersion method of distraction to control experimental ischemic pain,” The Israel Medical Association J. (IMAJ), Vol.8, Issue 4, pp. 261-265, 2006.
- [11] H. G. Hoffman, A. Garcia-Palacios, V. Kapa, J. Beecher, and S. R. Sharar, “Immersive virtual reality for reducing experimental ischemic pain,” Int. J. of Human-Computer Interaction, Vol.15, Issue 3, pp. 469-486, 2003.
- [12] L. M. Dahlquist, K. E. Weiss, L. Dillinger Clendaniel, E. F. Law, C. S. Ackerman, and K. D. McKenna, “Effects of videogame distraction using a virtual reality type head-mounted display helmet on cold pressor pain in children,” J. of Pediatric Psychology, Vol.34, Issue 5, pp. 574-584, 2008.
- [13] C. E. Rutter, L. M. Dahlquist, and K. E. Weiss, “Sustained efficacy of virtual reality distraction,” The J. of Pain, Vol.10, Issue 4, pp. 391-397, 2009.
- [14] N. Demeter, N. Josman, E. Eisenberg, and D. Pud, “Who can benefit from virtual reality to reduce experimental pain? A crossover study in healthy subjects,” European J. of Pain, Vol.19, Issue 10, pp. 1467-1475, 2015.
- [15] M. Höfle, M. Hauck, A. K. Engel, and D. Senkowski, “Viewing a needle pricking a hand that you perceive as yours enhances unpleasantness of pain,” Pain, Vol.153, Issue 5, pp. 1074-1081, 2012.
- [16] A. Bauer, J. Hagenburger, T. Plank, V. Busch, and M. W. Greenlee, “Mechanical pain thresholds and the rubber hand illusion,” Frontiers in Psychology, Vol.9, p. 712, 2018.
- [17] N. Matsunaga, A. T. Zengin, H. Okajima, and S. Kawaji, “Emulation of Fast and Slow Pains Using Multi-Layer Sensor Modeled the Layered Structure of Human Skin,” J. Robot. Mechatron., Vol.23, No.1, pp. 173-179, 2011.
- [18] J. Nishida, H. Takatori, K. Sato, and K. Suzuki, “CHILDHOOD: wearable suit for augmented child experience,” Proc. of the 2015 Virtual Reality Int. Conf., pp. 1-4, 2015.
- [19] D. Banakou, R. Groten, and M. Slater, “Illusory ownership of a virtual child body causes overestimation of object sizes and implicit attitude changes,” Proc. of the National Academy of Sciences, Vol.110, No.31, pp. 12846-12851, 2013.
- [20] A. Tajadura-Jiménez, D. Banakou, N. Bianchi-Berthouze, and M. Slater, “Embodiment in a Child-Like Talking Virtual Body Influences Object Size Perception, Self-Identification, and Subsequent Real Speaking,” Scientific Reports, Vol.7, No.1, pp. 1-12, 2017.
- [21] T. Kosaka, H. Misumi, T. Iwamoto, R. Songer, and J. Akita, “‘Mommy Tummy’ a pregnancy experience system simulating fetal movement,” ACM SIGGRAPH 2011 Emerging Technologies, pp. 1-1, 2011.
- [22] T. C. Peck, S. Seinfeld, S. M. Aglioti, and M. Slater, “Putting yourself in the skin of a black avatar reduces implicit racial bias,” Consciousness and Cognition, Vol.22, Issue 3, pp. 779-787, 2013.
- [23] L. Maister, M. Slater, M. V. Sanchez-Vives, and M. Tsakiris, “Changing bodies changes minds: owning another body affects social cognition,” Trends in Cognitive Sciences, Vol.19, pp. 6-12, 2015.
- [24] B. Philippe, D. Gonzalez-Franco, A. Pointeau, and C. Cherene, “The Machine to be Another – Embodied Telepresence using human performers,” 8th ACM Int. Conf. on Tangible, Embedded and Embodied Interaction (TEI 2014), 2014.
- [25] E. C. D. Oliveira, P. Bertrand, M. E. R. Lesur, P. Palomo, M. Demarzo, A. Cebolla, R. Baños, and R. Tori, “Virtual Body Swap: A New Feasible Tool to Be Explored in Health and Education,” 2016 XVIII Symp. on Virtual and Augmented Reality (SVR), pp. 81-89, 2016.
- [26] M. F. Yam, Y. C. Loh, C. S. Tan, S. Khadijah Adam, N. Abdul Manan, and R. Basir, “General Pathways of Pain Sensation and the Major Neurotransmitters Involved in Pain Regulation,” Int. J. of Molecular Sciences, Vol.19, Issue 8, p. 2164, 2018.
- [27] D. D. Price, J. W. Hu, R. Dubner, and R. H. Gracely, “Peripheral suppression of first pain and central summation of second pain evoked by noxious heat pulses,” Pain, Vol.3, Issue 1 pp. 57-68, 1977.
- [28] G. D. Simons and S. Mense, “Understanding and measurement of muscle tone as related to clinical muscle pain,” Pain, Vol.75, Issue 1, pp. 1-17, 1998.
- [29] M. Armour, K. Parry, N. Manohar, K. Holmes, T. Ferfolja, C. Curry, F. MacMillan, and C. A. Smith, “The Prevalence and Academic Impact of Dysmenorrhea in 21,573 Young Women: A Systematic Review and Meta-Analysis,” J. of Women’s Health (Larchmt), Vol.28, Issue 8, pp. 1161-1171, 2019.
- [30] M. Y. Dawood, “Primary dysmenorrhea: advances in pathogenesis and management,” Obstet Gynecol, Vol.108, Issue 2, pp. 428-441, 2006.
- [31] V. R. Pickles, “Prostaglandins and dysmenorrhea. Historical survey,” Acta Obstetricia et Gynecologica Scandinavica, Vol.58, Issue sup87, pp. 7-12, 1979.
- [32] J. L. Mason and N. A. M. MacKay, “Pain Sensations Associated with Electrocutaneous Stimulation,” IEEE Trans. on Biomedical Engineering, Vol.BME-23, No.5, pp. 405-409, 1976.
- [33] R. Melzack, “The McGill Pain Questionnaire: major properties and scoring methods,” Pain, Vol.1, Issue 3, pp. 277-299, 1975.
- [34] H. Kajimoto, “Electrotactile Display with Real-Time Impedance Feedback Using Pulse Width Modulation,” IEEE Trans. on Haptics, Vol.5, No.2, pp. 184-188, 2012.
- [35] J. Rosell, J. Colominas, P. Riu, R. Pallas-Areny, and J. G. Webster, “Skin impedance from 1 Hz to 1 MHz,” IEEE Trans. on Biomedical Engineering, Vol.35, No.8, pp. 649-651, 1988.
- [36] M. Isobe and C. Ishii, “Development of Two-Sensation Feedback Device for Myoelectric Prosthetic Hand Users – Compensation of Effect of Temperature Change on Haptic Feedback –,” J. Robot. Mechatron., Vol.32, No.1, pp. 199-208, 2020.
- [37] Y. Tamura, H. Ohtani, T. Umetani, and H. Nakamura, “Haptization on Numerical Simulation of Plasma,” IEEE Trans. on Plasma Science, Vol.38, No.10, pp. 2974-2979, 2010.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.