Paper:
Effectiveness of Continuous Grip Strength Measurement Using Social Assistive Robots on Older Adults at Home
Mio Nakamura*1,*2, Kohki Okajima*1, Yoshio Matsumoto*1,*3, Tomoki Tanaka*2, Katsuya Iijima*2,*4, and Misato Nihei*1,*2
*1Graduate School of Frontier Sciences, The University of Tokyo
5-1-5 Kashiwanoha, Kashiwa, Chiba 277-5859, Japan
7-3-1 Hongo, Bunkyo-ku, Tokyo 113-8656, Japan
6-2-3 Kashiwanoha, Kashiwa, Chiba 277-0882, Japan
*4Institute for Future Initiatives, The University of Tokyo
7-3-1 Hongo, Bunkyo-ku, Tokyo 113-0033, Japan
In this study, the effect of social assistive robots (SARs) on the continuity of health management activities was verified through the measurement of daily grip strength. We proposed and developed an intervention system for grip strength measurement and installed it in a SAR. Then, 23 older adults used the system at home with and without a SAR. Each setup was applied for three weeks and the rates at which the participants forgot their daily grip strength measurements were compared at the end of the period. The rates at which the daily measurements were forgotten decreased significantly when a SAR was used. In particular, 9 participants were able to decrease their rate of forgotten measurements after they used a SAR. Thus, the SAR enabled the participants to regularly perform grip strength measurement activities. These findings indicate that appropriate intervention measures using SARs are effective in promoting the continuity of daily healthcare activities of older adults living at home.
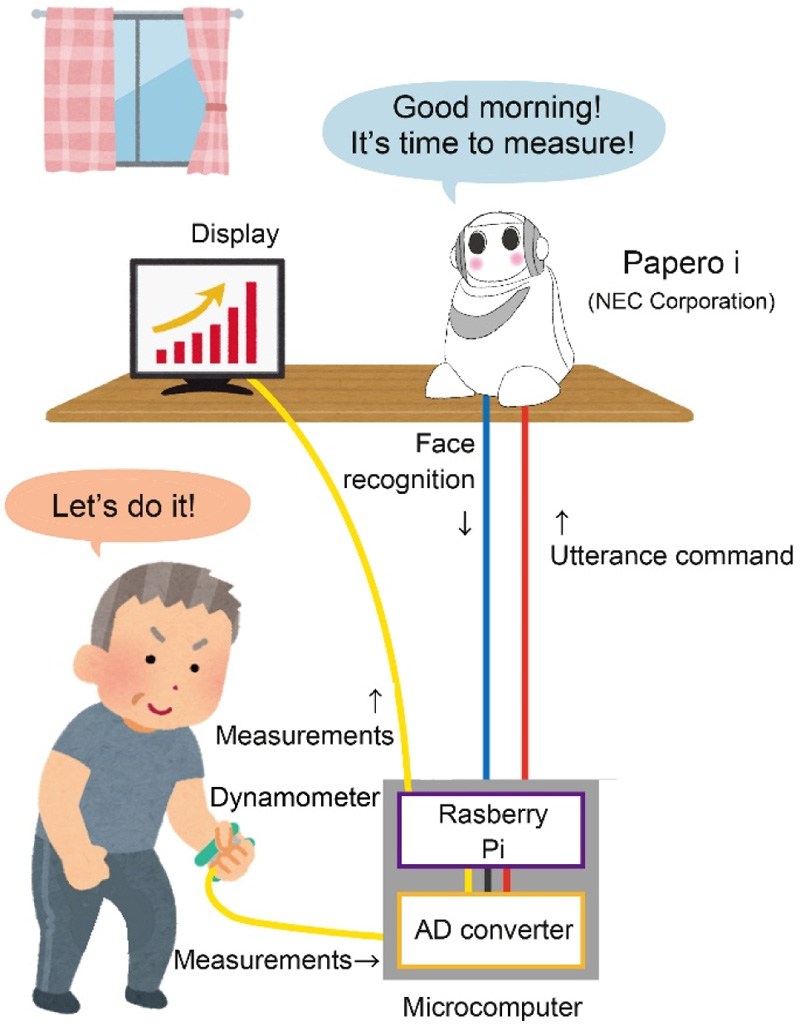
Concept of intervention system for grip strength measurement
- [1] D. Feil-Seifer and M. J. Mataric, “Defining socially assistive robotics,” 9th Int. Conf. Rehabil. Robot., pp. 465-468, 2005.
- [2] J. Abdi, A. Al-Hindawi, T. Ng, and M. P. Vizcaychipi, “Scoping review on the use of socially assistive robot technology in elderly care,” BMJ Open, Vol.8, e018815, 2018.
- [3] E. A. G. Jensen, J. Smith, and C. R. Kovach, “Social robots, robotic assistants, and home health monitoring devices: A gerontological research perspective,” Res. Gerontol. Nursing, Vol.12, No.4, pp. 163-166, 2019.
- [4] T. Inoue, M. Nihei, T. Narita, M. Onoda, R. Ishiwata, I. Mamiya, M. Shino, H. Kojima, S. Ohnaka, Y. Fujita, and M. Kamata, “Field-based development of an information support robot for persons with dementia,” Technol. Disability, Vol.24, No.4, pp. 263-271, 2012.
- [5] Y. Nishiura, T. Inoue, and M. Nihei, “Appropriate talking pattern of an information support robot for people living with dementia: a case study,” J. Assistive Technol., Vol.8, No.4, pp. 177-187, 2014.
- [6] T. W. Bickmore, K. Pusker, E. A. Schlenk, L. M. Pfeifer, and S. Sereika, “Maintaining reality: Relational agents for antipsychotic medication adherence. Interacting with Computers, Supportive Interaction,” Comput. Interventions Ment. Health, Vol.22, No.4, pp. 276-288, 2010.
- [7] M. Gonzales and L. Riek, “A social robotic aide for medication adherence,” Int. Conf. Pervasive Technol. Assistive Environ., pp. 1-4, 2012.
- [8] R. A. C. O. Keizer, L. V. Velsen, M. Moncharmont, B. Riche, N. Ammour, S. D. Signore, G. Zia, H. Hermens, and A. N’Dja, “Using socially assistive robots for monitoring and preventing frailty among older adults: a study on usability and user experience challenges,” Health Technol., Vol.9, pp. 595-605, 2019.
- [9] K. Obayashi and S. Masuyama, “The effects of introducing communicative robots with infra-red radiation monitoring system on night shift duties of nursing facility care worker,” J. of the Robotics Society of Japan, Vol.36, No.8, pp. 537-542, 2018.
- [10] K. Obayashi, N. Kodate, and S. Masuyama, “Measuring the impact of age, gender and dementia on communication-robot interventions in residential care homes,” Geriatr. Gerontol. Int., Vol.20, No.4, pp. 373-378, 2020.
- [11] S. Suzumura, E. Takano, Y. Sugishima, R. Narukawa, I. Makino, T. Abiko, S. Oi, and I. Kondo, “Reduced family care burden by using a communication robot: Case report,” Geriatr. Gerontol. Int., Vol.20, No.4, pp. 384-385, 2020.
- [12] M. Nakamura, M. Nihei, N. Kato, and T. Inoue, “Impact of the introduction of a verbal socially assistive robot on the relationship between older people and their caregivers in a nursing home,” SN Appl. Sci., Vol.2, 1657, 2020.
- [13] M. T. Chu, R. Khosla, S. M. S. Khaksar, and K. Nguyen, “Service innovation through social robot engagement to improve dementia care quality,” Assistive Technol., Vol.29, No.1, pp. 8-18, 2017.
- [14] C. Papadopoulos, T. Hill, L. Battistuzzi, N. Castro, A. Nigath, G. Randhawa, L. Merton, S. Kanoria, H. Kamide, N. Y. Chong, D. Hewson, R. Davidson, and A. Sgorbissa, “The CARESSES study protocol: testing and evaluating culturally competent socially assistive robots among older adults residing in long term care homes through a controlled experimental trial,” Arch. Public Health, Vol.78, 26, 2020.
- [15] M. Takahashi, K. Horiguchi, and K. Takamura, “A basic study of finger power: the measurement of strength and gripping power of fingers,” Meiwa Gakuen Junior Collegech Strength Bulletin, Vol.21, pp. 77-80, 2011.
- [16] N. Ikeda, S. Murata, H. Otao, Y. Kai, J. Murata, K. Tominaga, and K. Mizota, “Relationship between grip and physical function in the elderly,” West Kyusyu J. Rehabil. Sci., Vol.3, pp. 23-26, 2020 (in Japanese).
- [17] C. Celis-Morales, P. Welsh, D. M. Lyall, L. Steel, F. Petermann-Rocha, J. Anderson, S. Iliodromiti, A. Sillars, N. Graham, D. F. Mackay, J. P. Pell, J. M. R. Gill, N. Sattar, and S. Gray, “Associations of grip strength with cardiovascular, respiratory, and cancer outcomes and all cause mortality,” Br. Med. J., Vol.361, pp. 1-10, 2018.
- [18] D. P. Leong, K. K. Teo, S. Rangarajan, P. Lopez-Jaramillo, A. Avezum Jr., A. Orlandini, P. Seron, S. H. Ahmed, A. Rosengren, R. Kelishadi, O. Rahman, S. Swaminathan, R. Iqbal, R. Gupta, S. A. Lear, A. Oguz, K. Yusoff, K. Zatonska, J. Chifamba, E. Igumbor, V. Mohan, R. M. Anjana, H. Gu, W. Li, and S. Yusuf, “Prognostic value of grip strength: findings from the Prospective Urban Rural Epidemiology (PURE) study,” The Lancet, Vol.386, No.9990, pp. 266-273, 2015.
- [19] G. Viscogliosi, M. G. D. Bernardo, E. Ettorre, and I. M. Chiriac, “Handgrip strength predicts longitudinal changes in clock drawing test performance,” J. Nutr. Health Aging, Vol.21, No.5, pp. 593-596, doi: 10.1136/bmj.k1651, 2017.
- [20] L. P. Fried, C. M. Tangen, J. Waltston, A. B. Newman, C. Hirsch, J. Gottdiener, T. Seeman, R. Tracy, W. J. Kop, G. Burke, and M. A. McBurnie, “Frailty in older adults: Evidence for a phenotype,” J. Gerontol. A Biol. Sci. Med. Sci., Vol.56A, No.3, pp. 146-156, 2001.
- [21] K. Okajima, M. Nihei, M. Nakamura, Y. Matsumoto, T. Tanaka, K. Iijima, and M. Kamata, “Proposal of a supporting system of measuring grip strength continuously for health management of elderly people at home,” SICE Syetem Integration Division, 2020 (in Japanese).
- [22] B. Fogg, “Persuasive technology,” Nikkei Business Publications, Inc., 2005.
- [23] K. Nakagawa, K. Shinozawa, R. Matsumura, H. Ishigura, and N. Hagita, “Persuasive effects of robots’ personality,” Proc. of Forum on Informat. Technol., pp. 89-92, 2010 (in Japanese).
- [24] C. D. Kidd, “Designing for long-term human-robot interaction and application to weight loss,” Doctor of Philosophy in Media Arts and Sciences, Massachusetts Institute of Technology, 2008.
- [25] S. A. Beebe, “Eye-contact: A nonverbal determinant of speaker credibility,” Speech Teacher, Vol.23, pp. 21-25, 1974.
- [26] G. Breed, “The effect of intimacy: Reciprocity of retreat,” Br. J. Soc. Clin. Psychol., Vol.11, pp. 135-142, 1972.
- [27] M. B. LaCrosse, “Nonverbal behavior and perceived counselor attractiveness and persuasiveness,” J. Couns. Psychol., Vol.22, pp. 563-566, 1975.
- [28] M. Argyle, L. Lefebvre, and M. Cook, “The meaning of five patterns of gaze,” Eur. J. Soc. Psychol., Vol.4, pp. 125-136, 1974.
- [29] M. Nihei, Y. Nishiura, I. Mamiya, H. Kojima, K. Sadohara, S. Ohnaka, M. Kamata, and T. Inoue, “Change in the relationship between the elderly and information support robot system living together,” ITAP 2017: Human Aspects of IT for the Aged Population. Applications, Services and Contexts, pp. 433-442, 2017.
- [30] H. Kelman, “Processes of opinion change,” Public Opin. Q., Vol.25, No.1, pp. 57-78, 1961.
- [31] J. O. Prochaska and W. F. Velicer, “The transtheoretical model of health behavior change,” Am. J. Health Promot., Vol.12, No.1, pp. 38-48, 1997.
- [32] A. Bandura, “Self-Efficacy: The Exercise of Control,” W. H. Freeman, New York, 1997.
- [33] R. Gockley et al., “Designing robots for long-term social interaction,” 2005 IEEE/RSJ Int. Conf. on Intelligent Robots and Systems, pp. 1338-1343, 2005.
- [34] T. Kanda, T. Hirano, D. Eaton, and H. Ishiguro, “Interactive robots as social partners and peer tutors for children: a field trial,” Hum.-Comput. Interact., Vol.19, No.1, pp. 61-84, 2004 (in Japanese).
- [35] N. Hasegawa, H. Mani, K. Takeda, M. Sakuma, and N. Hasegawa, “Different effects of motor learning between visual and auditory feedback exercises in dynamic postural balance,” J. Jpn. Phys. Ther. Assoc., Vol.42, No.6, pp. 474-479, 2015 (in Japanese).
- [36] R. Ronsse, V. Puttemans, J. P. Coxon, D. J. Goble, J. Wagemans, N. Wenderoth, and S. P. Swinnen, “Motor learning with augmented feedback: modality-dependent behavioral and neural consequences,” Cereb. Cortex, Vol.21, pp. 1283-1294, 2011.
- [37] Y. Yoshizawa, “Emotional Control Techniques for Work,” CCC Medhia house, ISBN: 9784484132013, 2013 (in Japanese).
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.