Paper:
Evaluation of Walking Balance Based on Pose Difference Between Normal Walking and Walking Under Multi-Task Conditions
Hiroyuki Maeda, Miho Shogenji, and Tetsuyou Watanabe
Kanazawa University
Kakuma-machi, Kanazawa 920-1192, Japan
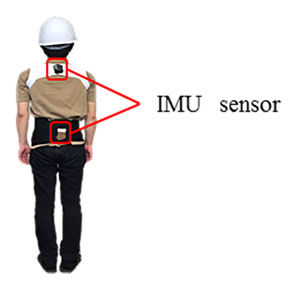
Appearance of a subject
- [1] S. N. Robinovitch, F. Feldman, Y. Yang, R. Schonnop, P. M. Leung, T. Sarraf, J. Sims-Gould, and M. Loughin, “Video capture of the circumstances of falls in elderly people residing in long-term care: an observational study,” Lancet, Vol.381, No.9860, pp. 47-54, 2013.
- [2] Y. Mano and R. Nakane, “Factors of the impaired walking and the fall of elderly people (in Japanese),” J. Clin. Rehabil., No.7, pp. 243-247, 1998.
- [3] “Comprehensive Survey of Living Conditions 2013,” Minist. Heal. Labour Welf., 2013 (in Japanese).
- [4] R. L. Gajdosik, D. W. Vander Linden, and A. K. Williams, “Influence of age on concentric isokinetic torque and passive extensibility variables of the calf muscles of women,” Eur. J. Appl. Physiol. Occup. Physiol., Vol.74, No.3, pp. 279-86, 1996.
- [5] T. Ghanavati, M. Salavati, N. Karimi, H. Negahban, I. Ebrahimi Takamjani, M. Mehravar, and M. Hessam, “Intra-limb coordination while walking is affected by cognitive load and walking speed,” J. Biomech., Vol.47, No.10, pp. 2300-2305, 2014.
- [6] S. R. Lord and R. C. Fitzpatrick, “Choice Stepping Reaction Time?: A Composite Measure of Falls Risk in Older People,” J. Gerontol. Med. Sci., Vol.56, No.10, pp. 627-632, 2001.
- [7] I. Melzer and L. I. E. Oddsson, “The Effect of a Cognitive Task on Voluntary Step Execution in Healthy Elderly and Young Individuals,” J. Am. Geriatr. Soc., Vol.52, No.10, pp. 1255-1262, 2004.
- [8] P. Mirjam, D. Kim, S. L. Daina, and S. R. Lord, “The association between choice stepping reaction time and falls in older adults – a path analysis model,” Age Ageing, Vol.39, No.10, pp. 99-104, 2010.
- [9] I. Melzer, I. Kurz, D. Shahar, M. Levi, and L. Oddsson, “Application of the voluntary step execution test to identify elderly fallers,” Age Ageing, Vol.36, No.10, pp. 532-537, 2007.
- [10] L. Lundin-Olsson, L. Nyberg, and Y. Gustafson, “Stops walking when talking’ as a predictor of falls in elderly people,” Lancet, Vol.349, No.9052, p. 617, 1997.
- [11] M. Yamada, H. Tanaka, S. Mori, K. Nagai, K. Uemura, B. Tanaka, T. Aoyama, and N. Ichihashi, “Fallers choose an early transfer gaze strategy during obstacle avoidance in dual-task condition,” Aging Clin. Exp. Res., Vol.23, No.4, pp. 316-319, 2011.
- [12] P. Silsupadol, A. Shumway-Cook, V. Lugade, P. van Donkelaar, L. S. Chou, U. Mayr, and M. H. Woollacott, “Effects of Single-Task Versus Dual-Task Training on Balance Performance in Older Adults: A Double-Blind, Randomized Controlled Trial,” Arch. Phys. Med. Rehabil., Vol.90, No.3, pp. 381-387, 2009.
- [13] O. Beauchet, C. Annweiler, V. Dubost, G. Allali, R. W. Kressig, S. Bridenbaugh, G. Berrut, F. Assal, and F. R. Herrmann, “Stops walking when talking: a predictor of falls in older adults?,” Eur. J. Neurol., No.7, pp. 786-795, 2009.
- [14] A. Shumway-Cook, M. Woollacott, K. a Kerns, and M. Baldwin, “The Effects of Two Types of Cognitive Tasks on Postural Stability in Older Adults With and Without a History of Falls,” J. Gerontol. Ser. A Biol. Sci. Med. Sci., Vol.52A, No.4, pp. M232-M240, 1997.
- [15] M. Woollacott and A. Shumway-Cook, “Attention and the control of posture and gait: a review of an emerging area of research,” Gait Posture, Vol.16, No.1, pp. 1-14, 2002.
- [16] J. Howcroft, J. Kofman, and E. D. Lemaire, “Review of fall risk assessment in geriatric populations using inertial sensors,” J. Neuroeng. Rehabil., pp. 1-12, 2013.
- [17] D. M. Karantonis, M. R. Narayanan, M. Mathie, N. H. Lovell, and B. G. Celler, “Implementation of a Real-Time Human Movement Classifier Using a Triaxial Accelerometer for Ambulatory Monitoring,” IEEE Trans. Inf. Technol. Biomed., Vol.10, No.1, pp. 156-167, 2006.
- [18] R. Moe-Nilssen and J. L. Helbostad, “Estimation of gait cycle characteristics by trunk accelerometry,” J. Biomech., Vol.37, No.1, pp. 121-126, 2004.
- [19] A. V. Rowlands and V. H. Stiles, “Accelerometer counts and raw acceleration output in relation to mechanical loading,” J. Biomech., Vol.45, No.3, pp. 448-454, 2012.
- [20] M. Mancini, A. Salarian, P. Carlson-Kuhta, C. Zampieri, L. King, L. Chiari, and F. B. Horak, “ISway: a sensitive, valid and reliable measure of postural control,” J. Neuroeng. Rehabil., Vol.9, No.1, p. 59, 2012.
- [21] S. Schmid, R. Hilfiker, and L. Radlinger, “Reliability and validity of trunk accelerometry-derived performance measurements in a standardized heel-rise test in elderly subjects,” J. Rehabil. Res. Dev., Vol.48, No.9, p. 1137, 2011.
- [22] H. Yack and R. Berger, “Dynamic stability in the elderly: identifying a possible measure,” J. Gerontol., Vol.48, No.5, pp. 225-230, 1993.
- [23] J. J. Kavanagh and H. B. Menz, “Accelerometry?: A technique for quantifying movement patterns during walking,” Vol.28, No.1, pp. 1-15, 2008.
- [24] C. Mizuike, S. Ohgi, and S. Morita, “Analysis of stroke patient walking dynamics using a tri-axial accelerometer,” Gait Posture, Vol.30, No.1, pp. 60-64, 2009.
- [25] H. B. Menz, S. R. Lord, and R. C. Fitzpatrick, “Age-related differences in walking stability,” Age Ageing, Vol.32, No.2, pp. 137-142, 2003.
- [26] S. O. H. Madgwick, A. J. L. Harrison, and R. Vaidyanathan, “Estimation of IMU and MARG orientation using a gradient descent algorithm,” 2011 IEEE Int. Conf. on Rehabilitation Robotics, pp. 1-7, 2011.
- [27] D. Comotti and M. Ermidoro, “REPORT OF THE COURSE PROGETTO DI MICROELETTRONICA English reduced version,” 9-Dof, 2011.
- [28] M. Schmid, A. Nardone, A. M. De Nunzio, M. Schmid, and M. Schieppati, “Equilibrium during static and dynamic tasks in blind subjects: no evidence of cross-modal plasticity,” Brain, Vol.130, No.8, pp. 2097-2107, 2007.
- [29] M. Yamada, B. Tanaka, K. Nagai, T. Aoyama, and N. Ichihashi, “Rhythmic stepping exercise under cognitive conditions improves fall risk factors in community-dwelling older adults: Preliminary results of a cluster-randomized controlled trial,” Aging Ment. Health, Vol.15, No.5, pp. 647-653, 2011.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.