Research Paper:
Development of a Living Laboratory to Verify Assistive Technology in Simulated Indoor and Outdoor Spaces
Kenji Kato*1,†
 , Tatsuya Yoshimi*1
, Tatsuya Yoshimi*1
 , Daiki Shimotori*2
, Daiki Shimotori*2
 , Keita Aimoto*3, Naoki Itoh*3, Kohei Okabe*4, Naoyuki Kubota*5
, Keita Aimoto*3, Naoki Itoh*3, Kohei Okabe*4, Naoyuki Kubota*5
 , Yasuhisa Hirata*6
, Yasuhisa Hirata*6
 , and Izumi Kondo*7
, and Izumi Kondo*7

*1Laboratory of Clinical Evaluation with Robotics, Assistive Robot Center, National Center for Geriatrics and Gerontology
7-430 Morioka-cho, Obu, Aichi 474-8511, Japan
†Corresponding author
*2Laboratory of Practical Technology in Community, Assistive Robot Center, National Center for Geriatrics and Gerontology
7-430 Morioka-cho, Obu, Aichi 474-8511, Japan
*3Department of Rehabilitation Medicine, National Center for Geriatrics and Gerontology
7-430 Morioka-cho, Obu, Aichi 474-8511, Japan
*4Mechanical System Safety Research Group, National Institute of Occupational Safety and Health, Japan Japan Organization of Occupational Health and Safety
1-4-6 Umezono, Kiyose, Tokyo 204-0024, Japan
*5Department of Mechanical Systems Engineering, Graduate School of Systems Design, Tokyo Metropolitan University
6-6 Asahigaoka, Hino, Tokyo 191-0065, Japan
*6Department of Robotics, Tohoku University
6-6-1 Aoba, Aramaki, Aoba-ku, Sendai, Miyagi 980-8579, Japan
*7Assistive Robot Center, National Center for Geriatrics and Gerontology
7-430 Morioka-cho, Obu, Aichi 474-8511, Japan
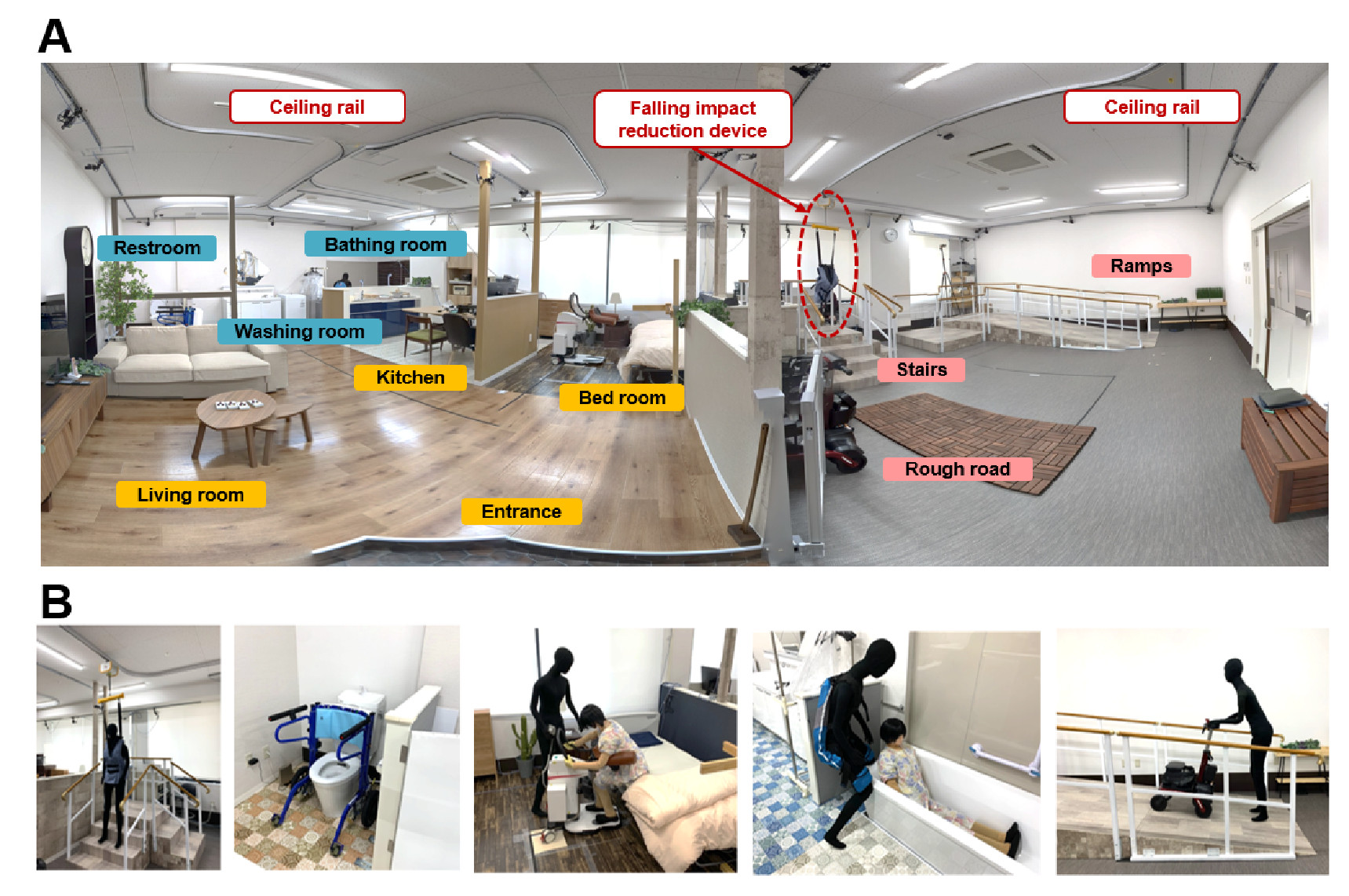
Assistive robots and technologies can play a key role in supporting the independence and social participation of older people, helping them living healthy lives and reducing the burden on caregivers. To support the effective development of assistive robots and technologies, it is important to develop a “living laboratory” to verify and adapt technology in real-life living spaces. The purpose of this study is to validate assistive robots using a living laboratory that simulates typical indoor and outdoor real-life situations. The rationale is to enable evaluation of daily living activities of older people in a simulated living space. To minimize the risk of trauma after falls, a ceiling suspension system was installed in the living laboratory. Six different commercially available mobility and transfer support robots were introduced and tested. We demonstrated that effective scenarios could be implemented using these assistive robots within the living laboratory. We implemented a 3D markerless motion capturing system in the outdoor space and showed that outdoor activities, including walking up and down a ramp, could be verified with sufficient accuracy in three cases: (i) normal use without a robot, (ii) use of the ceiling suspension system, and (iii) use of a mobility support robot on three healthy subjects. These results suggest that the proposed living laboratory can support testing and verification of assistive robots in simulated living environments.
Living laboratory to verify assistive technology
- [1] I. Kondo, “Frailty in an aging society and the applications of robots,” Japanese J. of Comprehensive Rehabilitation Science, Vol.10, pp. 47-49, 2019. https://doi.org/10.11336/jjcrs.10.47
- [2] D. A. Lindeman et al., “Technology and caregiving: Emerging interventions and directions for research,” The Gerontologist, Vol.60, No.Supplement_1, pp. S41-S49, 2020. https://doi.org/10.1093/geront/gnz178
- [3] T. Yoshimi et al., “Investigating proficiency using a lift-type transfer support device for effective care: Comparison of skilled and unskilled nursing homes,” Disability and Rehabilitation: Assistive Technology, 2022. https://doi.org/10.1080/17483107.2022.2128444
- [4] T. Yoshimi et al., “Increase of verbal communication by long-term use of transfer-support robots in nursing facilities,” Geriatrics & Gerontology Int., Vol.21, No.2, pp. 276-277, 2021. https://doi.org/10.1111/ggi.14113
- [5] K. Kato et al., “A rise-assisting robot extends life space and improves facial expressions of nursing home residents,” BMC Health Services Research, Vol.22, No.1, Article No.1588, 2022. https://doi.org/10.1186/s12913-022-08952-w
- [6] K. Kato et al., “Reduction of multiple-caregiver assistance through the long-term use of a transfer support robot in a nursing facility,” Assistive Technology, Vol.35, No.3, pp. 271-278, 2022. https://doi.org/10.1080/10400435.2022.2039324
- [7] K. Kato et al., “Identification of care tasks for the use of wearable transfer support robots – an observational study at nursing facilities using robots on a daily basis,” BMC Health Services Research, Vol.21, No.1, Article No.652, 2021. https://doi.org/10.1186/s12913-021-06639-2
- [8] K. Kato et al., “Novel bathing assist device decreases the physical burden on caregivers and difficulty of bathing activity in care recipients: A pilot study,” Applied Sciences, Vol.12, No.19, Article No.10131, 2022. https://doi.org/10.3390/app121910131
- [9] K. L. Koay et al., “Living with robots: Investigating the habituation effect in participants’ preferences during a longitudinal human-robot interaction study,” Proc. of the 16th IEEE Int. Symp. on Robot and Human Interactive Communication (RO-MAN 2007), pp. 564-569, 2007. https://doi.org/10.1109/ROMAN.2007.4415149
- [10] L. Kunze et al., “Artificial Intelligence for Long-Term Robot Autonomy: A Survey,” IEEE Robotics and Automation Letters, Vol.3, No.4, pp. 4023-4030, 2018. https://doi.org/10.1109/LRA.2018.2860628
- [11] K. Dautenhahn, “Robots in the wild: Exploring human-robot interaction in naturalistic environments,” Interaction Studies, Vol.10, No.3, pp. 269-273, 2009. https://doi.org/10.1075/is.10.3.01dau
- [12] C. D. Kidd et al., “The aware home: A living laboratory for ubiquitous computing research,” Proc. of the 2nd Int. Workshop on Cooperative Buildings (CoBuild’99) – Integrating Information, Organizations, and Architecture, pp. 191-198, 1999. https://doi.org/10.1007/10705432_17
- [13] S. S. Intille et al., “A living laboratory for the design and evaluation of ubiquitous computing technologies,” CHI’05 Extended Abstracts on Human Factors in Computing Systems, pp. 1941-1944, 2005. https://doi.org/10.1145/1056808.1057062
- [14] D. D. Vaziri, “Exploring user experience and technology acceptance for a fall prevention system: Results from a randomized clinical trial and a living lab,” D. D. Vaziri, “Facilitating Daily Life Integration of Technologies for Active and Healthy Aging: Understanding Demands of Older Adults in Health Technology Design,” pp. 27-39, Springer, 2018. https://doi.org/10.1007/978-3-658-22875-0_5
- [15] H. Verbeek et al., “The living lab in ageing and long-term care: A sustainable model for translational research improving quality of life, quality of care and quality of work,” The J. of Nutrition, Health & Aging, Vol.24, No.1, pp. 43-47, 2020. https://doi.org/10.1007/s12603-019-1288-5
- [16] J. B. M. Colomer et al., “Experience in evaluating AAL solutions in living labs,” Sensors, Vol.14, No.4, Article No.4, 2014. https://doi.org/10.3390/s140407277
- [17] K. De Moor et al., “Proposed framework for evaluating quality of experience in a mobile, testbed-oriented living lab setting,” Mobile Networks and Applications, Vol.15, No.3, pp. 378-391, 2010. https://doi.org/10.1007/s11036-010-0223-0
- [18] K. Kato et al., “Design of a demonstration space, the ‘Living Lab,’ for monitoring daily activities in the older adult and the assessment of assistive technologies,” The 10th Int. Symp. on Computational Intelligence and Industrial Applications (ISCIIA2022), Session No.C2-4, 2022.
- [19] R. M. Kanko et al., “Inter-session repeatability of markerless motion capture gait kinematics,” J. of Biomechanics, Vol.121, Article No.110422, 2021. https://doi.org/10.1016/j.jbiomech.2021.110422
- [20] R. M. Kanko et al., “Assessment of spatiotemporal gait parameters using a deep learning algorithm-based markerless motion capture system,” J. of Biomechanics, Vol.122, Article No.110414, 2021. https://doi.org/10.1016/j.jbiomech.2021.110414
- [21] W. Hlauschek, P. Panek, and W. L. Zagler, “Involvement of elderly citizens as potential end users of assistive technologies in the living lab Schwechat,” Proc. of the 2nd Int. Conf. on Pervasive Technologies Related to Assistive Environments (PETRA’09), Article No.55, 2009. https://doi.org/10.1145/1579114.1579169
- [22] B. Krieg-Brückner et al., “Mobility assistance in the Bremen Ambient Assisted Living Lab,” GeroPsych, Vol.23, No.2, pp. 121-130, 2010. https://doi.org/10.1024/1662-9647/a000009
- [23] A. Teixeira et al., “A new living lab for usability evaluation of ICT and next generation networks for Elderly@Home,” Proc. of the 1st Int. Living Usability Lab Workshop on AAL Latest Solutions, Trends and Applications (AAL 2011), pp. 85-97, 2011. https://doi.org/10.5220/0003335000850097
- [24] H.-W. Huang et al., “Mobile robotic platform for contactless vital sign monitoring,” Cyborg and Bionic Systems, Vol.2022, Article No.9780497, 2022. https://doi.org/10.34133/2022/9780497
- [25] A. P. J. Zanardi et al., “Gait parameters of Parkinson’s disease compared with healthy controls: A systematic review and meta-analysis,” Scientific Reports. Vol.11, No.1, Article No.752, 2021. https://doi.org/10.1038/s41598-020-80768-2
- [26] M. McGrath et al., “The impact of three-dimensional gait analysis in adults with pathological gait on management recommendations,” Gait & Posture, Vol.105, pp. 75-80, 2023. https://doi.org/10.1016/j.gaitpost.2023.06.014
- [27] Q. Zhong et al., “Gait kinematic and kinetic characteristics of older adults with mild cognitive impairment and subjective cognitive decline: A cross-sectional study,” Frontiers in Aging Neuroscience, Vol.13, Article No.664558, 2021. https://doi.org/10.3389/fnagi.2021.664558
- [28] M. E. Tinetti et al., “A multifactorial intervention to reduce the risk of falling among elderly people living in the community,” The New England J. of Medicine, Vol.331, No.13, pp. 821-827, 1994. https://doi.org/10.1056/NEJM199409293311301
- [29] D. T. Wade and B. A. de Jong, “Recent advances in rehabilitation,” BMJ, Vol.320, No.7246, pp. 1385-1388, 2000. https://doi.org/10.1136/bmj.320.7246.1385
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.