Paper:
Evaluation of Tympanic Temperature, Heart Rate Variability and Finger-Foot Reaction Using VR in the Elderly
Yutaka Yoshida*,**, Itaru Kaneko**, Junichiro Hayano***, Kiyoko Yokoyama*, and Emi Yuda**
*Graduate School of Design and Architecture, Nagoya City University
2-1-10 Kita Chikusa, Chikusa-ku, Nagoya 464-0083, Japan
**Center for Data-Driven Science and Artificial Intelligence, Tohoku University
41 Kawauchi, Aoba-ku, Sendai 980-8576, Japan
***Heart Beat Science Lab Co., Ltd.
6-6-40 Aoba Aramaki, Aoba-ku, Sendai 980-0845, Japan
We evaluated tympanic temperatures, heart rate variability, as well as finger and foot reaction times in elderly using VR simulations of amusement park attractions. The subjects were 8 elderly people (mean age ± S.D., 75±7 year, range 61–85 year), including four females. A roller coaster, swing ride, and rotating cart were used for the amusement park attractions. Subjects were requested to wear VR headsets, rest for 3 minutes, and then were asked to run through the same virtual amusement ride 3 times in a row, which takes 3 minutes and 30 seconds. After another 3 minutes of resting, the subjects were requested to answer a simulator sickness questionnaire (SSQ). In addition, PVT and PS-PVT were performed before and after the attraction rides. Results showed that HRV were not significantly different, but time phase change of tympanic temperature showed increasing trend (P=0.095). As the results of SSQ, increasing trend of nausea was observed in roller coaster than rotating cart (P=0.097). The results of PVT and PS-PVT showed that finger reaction time was significantly faster after the swing ride (P=0.023) and foot reaction time was significantly faster after the rotating cart (P=0.034). It is considered that the tympanic temperature increases when VR sickness occurs. Work performance improved after using VR simulations of amusement park attractions. It is suggested that the moving stimulus of VR vehicles improves finger-foot reactivity and activates concentration in elderly people.
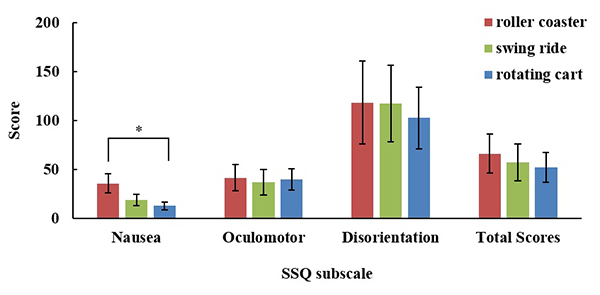
Evaluation of SSQ for VR amusement
- [1] S. Rutkowski, A. Rutkowska, P. Kiper et al., “Virtual Reality Rehabilitation in Patients with Chronic Obstructive Pulmonary Disease: A Randomized Controlled Trial,” Int. J. Chron. Obstruct. Pulmon. Dis., No.15, pp. 117-124, 2020.
- [2] J. A. Garcia, “A Virtual Reality Game-Like Tool for Assessing the Risk of Falling in the Elderly,” Stud. Health Technol. Inform., Vol.266, pp. 63-69, 2019.
- [3] S. Ohyama, S. Nishiike, H. Watanabe et al., “Autonomic responses during motion sickness induced by virtual reality,” Auris Nasus Larynx, Vol.34, Issue 3, pp. 303-306, 2007.
- [4] N. A. Webb and M. J. Griffin, “Eye Movement, Vection, and Motion Sickness with Foveal and Peripheral Vision,” Aviat. Space Environ. Med., Vol.74, No.6, pp. 622-625, 2003.
- [5] M. Oinuma, K. Hirayanagi, K. Yajima et al., “Changes in cardio-respiratory function, heart rate variability, and electrogastrogram preceding motion sickness-like symptoms induced by virtual reality stimulus,” Japanese J. of Aerospace and Environmental Medicine, Vol.41, No.3, pp. 99-109, 2004.
- [6] E. Nalivaiko, J. A. Rudd, and R. H. Y. So, “Motion sickness, nausea and thermoregulation: The “toxic” hypothesis,” Temperature, Vol.1, Issue 3, pp. 164-171, 2014.
- [7] H. G. Kim, H.-T. Lim, S. Lee et al., “VRSA Net: VR Sickness Assessment Considering Exceptional Motion for 360° VR Video,” IEEE Trans. Image Process, Vol.28, Issue 4, pp. 1646-1660, 2019.
- [8] D. Cho, J. Ham, J. Oh et al., “Detection of Stress Levels from Biosignals Measured in Virtual Reality Environments Using a Kernel-Based Extreme Learning Machine,” Sensors, Vol.17, Issue 10, Article No.2435, 2017.
- [9] X. Li, C. Zhu, C. Xu et al., “VR motion sickness recognition by using EEG rhythm energy ratio based on wavelet packet transform,” Computer Methods and Programs in Biomedicine, Vol.188, Article No.105266, 2020.
- [10] C. Nakagawa, M. Ohsuga, and T. Takeda, “Basic study toward VE-sickness assessment,” The Japan J. of Ergonomics, Vol.36, Issue 3, pp. 131-138, 2000.
- [11] J. Kim, W. Kim, S. Ahn et al., “Virtual reality sickness predictor: Analysis of visual-vestibular conflict and VR contents,” 10th Int. Conf. on Quality of Multimedia Experience (QoMEX), 2018.
- [12] D. E. Angelaki, E. M. Klier, and L. H. Snyder, “A Vestibular Sensation: Probabilistic Approaches to Spatial Perception,” Neuron, Vol.64, Issue 4, pp. 448-461, 2009.
- [13] N. Norouzi, G. Bruder, and G. Welch, “Assessing vignetting as a means to reduce VR sickness during amplified head rotations,” Proc. of the 15th ACM Symp. on Applied Perception (SAP’18), Article No.19, 2018.
- [14] H. G. Kim, W. J. Baddar, H.-T. Lim et al., “Measurement of exceptional motion in VR video contents for VR sickness assessment using deep convolutional autoencoder,” Proc. of the 23rd ACM Symp. on Virtual Reality Software and Technology (VRST’17), Article No.36, 2017.
- [15] P. Graw, K. Kräuchi, V. Knoblauch et al., “Circadian and wake-dependent modulation of fastest and slowest reaction times during the psychomotor vigilance task,” Physiol. Behav., Vol.80, Issue 5, pp. 695-701, 2004.
- [16] E. Yuda, Y. Yoshida, N. Ueda et al., “Effects of aging on foot pedal responses to visual stimuli,” J. of Physiological Anthropology, Vol.39, Article No.3, 2020.
- [17] J. Hayano, J. A. Taylor, A. Yamada et al., “Continuous assessment of hemodynamic control by complex demodulation of cardiovascular variability,” American J. of Physiology, Vol.264, Issue 4, pp. H1229-H1238, 1993.
- [18] S. Ohyama, S. Nishiike, H. Watanabe et al., “Autonomic responses during motion sickness induced by virtual reality,” Auris Nasus Larynx, Vol.34, Issue 3, pp. 303-306, 2007.
- [19] C. Kazzi, C. Blackmore, F. Shirbani et al., “Effects of instructed meditation augmented by computer-rendered artificial virtual environment on heart rate variability,” 40th Annual Int. Conf. of the IEEE Eng. Med. Biol. Soc. (EMBC), pp. 2768-2771, 2018.
- [20] H. Watanabe, W. Teramoto, and H. Umemura, “Effect of predictive sign of acceleration on heart rate variability in passive translation situation:preliminary evidence using visual and vestibular stimuli in VR environment,” J. Neuroeng. Rehabil., Vol.4, Article No.36, 2007.
- [21] Y. Yokota, M. Aoki, K. Mizuta et al., “Motion sickness susceptibility associated with visually induced postural instability and cardiac autonomic responses in healthy subjects,” Acta Oto-Laryngologica, Vol.125, No.3, pp. 280-285, 2005.
- [22] I. Doweck, C. R. Gordon, A. Shlitner et al., “Alternations in R-R variability associated with experimental motion sickness,” J. Auton. Nerv. Syst., Vol.67, Issue 1, pp. 31-37, 1997.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.