Paper:
PPG Signal Morphology-Based Method for Distinguishing Stress and Non-Stress Conditions
Solaiman Ahmed*,†, Tanveer Ahmed Bhuiyan**, and Manabu Nii*
*Graduate School of Engineering, University of Hyogo
2167 Shosha, Himeji, Hyogo 671-2280, Japan
**Demant A/S
9 Kongebakken, Smorum 2765, Denmark
†Corresponding author
In this study, the morphology of the PPG signal has been analyzed to be a potential cardiovascular marker for physiological stress. The morphology of the PPG signal was quantified as signal quality index by comparing the template beat (extracted from resting conditions) to the PPG beats recorded during vigorous physical activity. Data was taken from eight subjects where they performed some physical activities ranging from low to high intensity. It was found that, the mean and standard deviation of correlation coefficient between non-stress condition template beat and annotated PPG beat, 89.43±5.17 (%) and 44.23±10.48 (%) for non-stress and stress beat respectively with P value of 2.04*10-06 shows significantly difference between correlation coefficients (stress and non-stress). Whereas, mean and standard deviation of dynamic time warping correlation coefficients are 93.43±5.06 (%) and 85.93±4.18 (%) for non-stress and stress beat respectively with P value of .04. The morphology results corroborate the findings from the traditional HRV parameters generally used for stratifying stress.
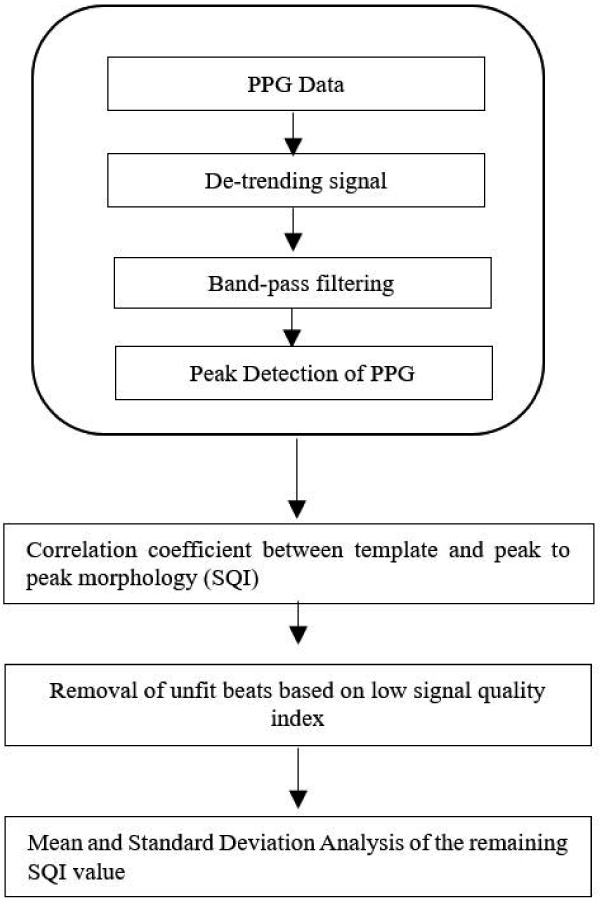
PPG morphology based stress estimation process
- [1] M. Campkin, “Stress management in primary care,” Family Practice, Vol.17, No.1, pp. 98-99, 2000.
- [2] J. F. Thayer, F. Åhs, M. Fredrikson, J. J. Sollers III, and T. D.Wager, “A meta-analysis of heart rate variability and neuroimaging studies: implications for heart rate variability as a marker of stress and health,” Neuroscience & Biobehavioral Reviews, Vol.36, No.2, pp. 747-756, 2012.
- [3] M. Elgendi, “Optimal signal quality index for photoplethysmogram signals,” Bioengineering, Vol.3, No.4, Article No.21, 2016.
- [4] S. Wolf, “The end of the rope: the role of the brain in cardiac death,” Canadian Medical Association J., Vol.97, No.17, p. 1022-1025, 1967.
- [5] G. G. Berntson, J. Thomas Bigger Jr., D. L. Eckberg et al., “Heart rate variability: origins, methods, and interpretive caveats,” Psychophysiology, Vol.34, No.6, pp. 623-648, 1997.
- [6] U. R. Acharya, K. P. Joseph, N. Kannathal, C. M. Lim, and J. S. Suri, “Heart rate variability: a review,” Medical and Biological Engineering and Computing, Vol.44, No.12, pp. 1031-1051, 2006.
- [7] M. Malik and A. J. Camm, “Heart rate variability,” Clinical cardiology, Vol.13, No.8, pp. 570-576, 1990.
- [8] J. Sztajzel, “Heart rate variability: a noninvasive electrocardiographic method to measure the autonomic nervous system,” Swiss Medical Weekly, Vol.134, Nos.35-36, pp. 514-522, 2004.
- [9] H.-G. Kim, E.-J. Cheon, D.-S. Bai, Y. H. Lee, and B.-H. Koo, “Stress and Heart Rate Variability: A Meta-Analysis and Review of the Literature,” Psychiatry Investig., Vol.15, No.3, pp. 235-245, 2018.
- [10] P. Celka, P. H. Charlton, B. Farukh, P. Chowienczyk, and J. Alastruey, “Influence of mental stress on the pulse wave features of photoplethysmograms,” Healthc. Technol. Lett., Vol.7, No.1, pp. 7-12, 2019.
- [11] H. Shin and S. D. Min, “Feasibility study for the non-invasive blood pressure estimation based on ppg morphology: normotensive subject study,” Biomed. Eng. Online, Vol.16, Article No.10, 2017.
- [12] N. A. Wisely and L. B. Cook, “Arterial flow waveforms from pulse oximetry compared with measured Doppler flow waveforms: apparatus,” Anaesthesia, Vol.56, No.6, pp. 556-561, 2001.
- [13] H. Takada, K. Washino, J. S. Harrell, and H. Iwata, “Acceleration plethysmography to evaluate aging effect in cardiovascular system, Using new criteria of four wave patterns,” Medical Progress Through Technology, Vol.21, No.4, pp. 205-210, 1996.
- [14] E. Yuda, M. Shibata, Y. Ogata et al., “Pulse rate variability: a new biomarker, not a surrogate for heart rate variability,” J. of Physiological Anthropology, Vol.39, Article No.21, 2020.
- [15] A. Reiss, I. Indlekofer, P. Schmidt, and K. van Laerhoven, “Deep PPG: Large-Scale Heart Rate Estimation with Convolutional Neural Networks,” Sensors, Vol.19, No.14, 3039, 2019.
- [16] U. Yadav, S. N. Abbas, and D. Hatzinakos, “Evaluation of PPG biometrics for authentication in different states,” Proc. of the 2018 Int. Conf. on Biometrics (ICB), pp. 277-282, 2018.
- [17] Task Force of the European Society of Cardiology, “Heart rate variability: standards of measurement, physiological interpretation and clinical use,” Circulation, Vol.93, pp. 1043-65, 1996.
- [18] R. E. Kleiger, P. K. Stein, M. S. Bosner, and J. N. Rottman, “Time domain measurements of heart rate variability,” Cardiology Clinics, Vol.10, No.3, pp. 487-498, 1992.
- [19] K. Hnatkova, X. Copie, A. Staunton, and M. Malik, “Numeric processing of Lorenz plots of R-R intervals from long-term ECGs: comparison with time-domain measures of heart rate variability for risk stratification after myocardial infarction,” J. of Electrocardiology, Vol.28, No.Supplement 1, pp. 74-80, 1995.
- [20] Z. Ori, G. Monir, J. Weiss, X. Sayhouni, and D. H. Singer, “Heart Rate Variability. Frequency Domain Analysis,” Cardiology Clinics, Vol.10, No.3, pp. 499-537, 1992.
- [21] A. Malliani, M. Pagani, F. Lombardi, and S. Cerutti, “Cardiovascular neural regulation explored in the frequency domain,” Circulation, Vol.84, No.2, pp. 482-492, 1991.
- [22] F. Shaffer and J. P. Ginsberg, “An Overview of Heart Rate Variability Metrics and Norms,” Front. Public Health, Vol.5, Article No.258, 2017.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.