Paper:
Health Vulnerability Index in Disaster Preparedness: An Analysis in the Cyclone Prone Blocks of Purba Medinipur, India
Sripurna Kanjilal*,†
 , Gupinath Bhandari**, and Souvik Majumder***
, Gupinath Bhandari**, and Souvik Majumder***
*School of Oceanographic Studies, Jadavpur University
188 Raja Subodh Chandra Mullick Road, Jadavpur, Kolkata, West Bengal 700032, India
†Corresponding author
**Department of Civil Engineering, Jadavpur University
Kolkata, India
***Department of Pharmacology, Medical College Kolkata
Kolkata, India
The Indian subcontinent has recently seen an increasingly high incidence of natural disasters, mainly cyclones resulting in loss of lives and property and damage to livelihood. Risk is defined by the negative effects of interactions between exposure, hazards, and vulnerable situations. The majority of the existing vulnerability indices emphasize social and economic vulnerability and often exclude the significance of health vulnerability. The study aims to compute a Health Vulnerability Index (HVI) in the research area of five cyclone-prone community development blocks in the Purba Medinipur district of West Bengal, India: Ramnagar-I, Ramnagar-II, Contai-I, Deshapran, and Khejuri-II. A three-phase methodology was used to develop the final disaster risk model. Phase 1: extensive literature review and identification of the relevant indicators: vulnerable population, disabled population, under-five mortality rate, unmet bed demand, unmet doctor demand, poor households, incidence of tuberculosis, vaccination gap, and measles vaccination gap, Phase 2: a two-stage dimension reduction statistical method to identify the weighing of the indicators, Phase 3: creates the final disaster risk by Risk = Exposure × Hazard × Vulnerability. Khejuri-II has the highest index of health vulnerability, which coupled with poor infrastructural facilities results in a high corresponding risk. Ramnagar-I being a hotbed of tourism and economic activities in the area poses the lowest HVI and hence the lowest risk. This proposed index which provides a judicious reflection of health vulnerability may serve as a policy and implementation tool to facilitate capacity building to improve resilience in the cyclone-affected areas.
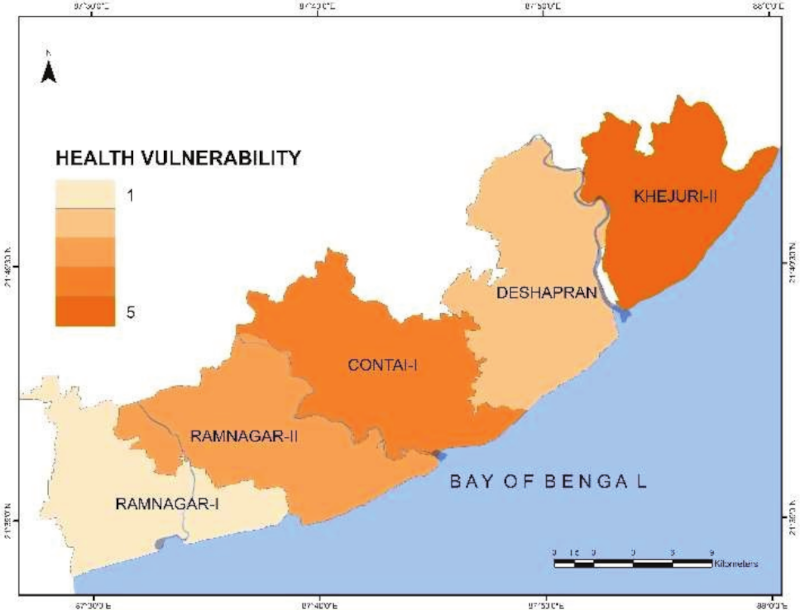
Health vulnerability of study area
- [1] D. K. Yadav and A. Barve, “Analysis of socioeconomic vulnerability for cyclone-affected communities in coastal Odisha, India,” Int. J. of Disaster Risk Reduction, Vol.22, pp. 387-396, 2017. https://doi.org/10.1016/j.ijdrr.2017.02.003
- [2] A. Chakraborty and P. K. Joshi, “Mapping disaster vulnerability in India using analytical hierarchy process,” Natural Hazards and Risk, Vol.7, Issue 1, pp. 308-325, 2016. https://doi.org/10.1080/19475705.2014.897656
- [3] S. Ghosh and B. Mistri, “Cyclone-induced coastal vulnerability, livelihood challenges and mitigation measures of Matla–Bidya inter-estuarine area, Indian Sundarban,” Natural Hazards, Vol.116, No.3, pp. 3857-3878, 2023. https://doi.org/10.1007/s11069-023-05840-2
- [4] C. B. Field, V. R. Barros, D. J. Dokken, K. J. Mach, M. D. Mastrandrea, T. E. Bilir, M. Chatterjee, K. L. Ebi, Y. O. Estrada, R. C. Genova, B. Girma, E. S. Kissel, A. N. Levy, S. MacCracken, P. R. Mastrandrea, and L. L. White (Eds.), “Climate Change 2014 Impacts, Adaptation, and Vulnerability Part A: Global and Sectoral Aspects Working Group Ii Contribution to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change,” Cambridge University Press, 2014. https://www.ipcc.ch/site/assets/uploads/2018/02/WGIIAR5-FrontMatterA_FINAL.pdf [Accessed December 25, 2023]
- [5] S. K. Dube, T. A. Mazumder, and A. R. Das, “An approach to vulnerability assessment for tropical cyclones: A case study of a coastal district in West Bengal,” ITPI J., Vol.3, No.4, pp. 15-27, 2006.
- [6] UNISDR, “2009 UNISDR terminology on disaster risk reduction,” 2009. https://www.undrr.org/publication/2009-unisdr-terminology-disaster-risk-reduction [Accessed May 29, 2023]
- [7] N. Brooks, “Vulnerability, risk and adaptation: A conceptual framework,” Tyndall Centre for Climate Change Research, Working Paper No.38, 2003.
- [8] B. Wisner, P. Blaikie, T Cannon, and I. Davis, “At Risk: Natural Hazards, People’s Vulnerability and Disasters,” Routledge, 2004. https://doi.org/10.4324/9780203714775
- [9] S. Sterlacchini, S. O. Akbas, J. Blahut, O. C. Mavrouli, C. Garcia, B. Q Luna, and J. Corominas, “Methods for the characterization of the vulnerability of elements at risk,” T. Van Asch, J. Corominas, S. Greiving, J.-P. Malet, and S. Sterlacchini (Eds.), “Mountain risks: From prediction to management and governance,” Advances in Natural and Technological Hazards Research, Vol.34, pp. 233-273, 2013. https://doi.org/10.1007/978-94-007-6769-0_8
- [10] K. I. Shoaf and S. J. Rotiman, “Public health impact of disasters,” Australian J. of Emergency Management, Vol.15, Issue 3, pp. 1324-1540, 2000. https://search.informit.org/doi/10.3316/ielapa.369826620745919
- [11] W. Kron, “Flood risk = hazard · values · vulnerability,” Water Int., Vol.30, Issue 1, pp. 58-68, 2005. https://doi.org/10.1080/02508060508691837
- [12] I. Kelman, “Lost for words amongst disaster risk science vocabulary?,” Int. J. of Disaster Risk Science, Vol.9, pp. 281-291, 2018. https://doi.org/10.1007/s13753-018-0188-3
- [13] A. Khan, S. Chatterjee, and D. Bisai, “Block level assessment of human vulnerability in Paschim Medinipur district, WB: Regional mapping of social contours quantitively,” J. of Business Management and Social Sciences Research, Vol.2, No.11, pp. 5-11, 2013.
- [14] E. Y. Chan, Z. Huang, H. C. Lam, C. K. Wong, and Q. Zou, “Health vulnerability index for disaster risk reduction: Application in Belt and Road Initiative (BRI) region,” Int. J. of Environmental Research and Public Health, Vol.16, Issue 3, Article No.380, 2019. https://doi.org/10.3390/ijerph16030380
- [15] N. Brooks, W. N. Adger, and P. M. Kelly, “The determinants of vulnerability and adaptive capacity at the national level and the implications for adaptation,” Global Environmental Change, Vol.15, Issue 2, Article No.151163, 2005. https://doi.org/10.1016/j.gloenvcha.2004.12.006
- [16] S. L. Cutter, B. J. Boruff, and W. L. Shirley, “Social vulnerability to environmental hazards,” Social Science Quarterly, Vol.84, No.2, pp. 242-261, 2003. https://doi.org/10.1111/1540-6237.8402002
- [17] J. Wang and L. Geng, “Effects of socioeconomic status on physical and psychological health: Lifestyle as a mediator,” Int. J. of Environmental Research and Public Health, Vol.16, Issue 2, Article No.281, 2019. https://doi.org/10.3390/ijerph16020281
- [18] Health Adaptation Plan for Cyclones. https://ncdc.mohfw.gov.in/WriteReadData/l892s/20047793071632477296.pdf [Accessed January 30, 2024]
- [19] D. D. Saulnier, K. B. Ribacke, and J. Von Schreeb, “No calm after the storm: A systematic review of human health following flood and storm disasters,” Prehospital and Disaster Medicine, Vol.32, No.5, pp. 568-579, 2017. https://doi.org/10.1017/S1049023X17001510
- [20] W. Huang, Y. Gao, R. Xu, Z. Yang, P. Yu, T. Ye, E. A. Ritchie, S. Li, and Y. Guo, “Health effects of cyclones: A systematic review and meta-analysis of epidemiological studies,” Environmental Health Perspectives, Vol.131, Issue 8, Article No.86001, 2023. https://doi.org/10.1289/EHP12158
- [21] S. Chatterjee and A. Kundu, “Assessing the north Indian maritime cyclonic turbulences with extraordinary reference to incredibly serious cyclonic tempest Fani: Meteorological inconstancy, India’s readiness with the awful consequences,” Preprint, Research Square, 2021. https://doi.org/10.21203/rs.3.rs-574592/v1
- [22] E. K. Noji, “Medical and Public Health Consequences of Natural and Biological Disasters,” Natural Hazards Review, Vol.2, No.3, pp. 143-156, 2001. https://doi.org/10.1061/(ASCE)1527-6988(2001)2:3(143)
- [23] S. H. Shin and H. Ji, “Health risks of natural hazards and resilience resources: Evidence from a U.S. nationwide longitudinal study,” Social Science and Medicine, Vol.281, Article No.114110, 2021. https://doi.org/10.1016/j.socscimed.2021.114110
- [24] S. Zahran, L. Peek, J. G. Snodgrass, S. Weiler, and L. Hempel, “Economics of disaster risk, social vulnerability, and mental health resilience,” Risk Analysis, Vol.31, Issue 7, pp. 1107-1119, 2011. https://doi.org/10.1111/j.1539-6924.2010.01580.x
- [25] J.-C. Lee, C.-P. Chang, and Y. Liao, “Capacity building for disaster risk reduction: A long-term program of the IRDR International Centre of Excellence at Taipei (ICoE-Taipei),” J. Disaster Res., Vol.18, No.7, pp. 691-699, 2023. https://doi.org/10.20965/jdr.2023.p0691
- [26] T. Hák, S. Janoušková, and B. Moldan, “Sustainable development goals: A need for relevant indicators,” Ecological Indicators, Vol.60, No.2, pp. 565-573, 2016. https://doi.org/10.1016/j.ecolind.2015.08.003
- [27] B. Dash and A. Walia, “Role of multi-purpose cyclone shelters in India: Last mile or neighbourhood evacuation,” Tropical Cyclone Research and Review, Vol.9, No.4, pp. 206-217, 2020. https://doi.org/10.1016/j.tcrr.2020.11.002
- [28] A. Almutairi, M. Mourshed, and R. F. Ameen, “Coastal community Resilience Frameworks for Disaster Risk Management,” Natural Hazards, Vol.101, No.2, pp. 595-630, 2020. https://doi.org/10.1007/s11069-020-03875-3
- [29] N. Mao, C. K. An, L. Y. Guo, M. Wang, L. Guo, S. R. Guo, and E. S. Long,, “Transmission risk of infectious droplets in physical spreading process at different times: A review,” Building and Environment, Vol.185, Article No.107307, 2020. https://doi.org/10.1016/j.buildenv.2020.107307
- [30] A. Misin, R. M. Antonello, S. Bella, G. Campisciano, N. Zanotta, D.R. Giacobbe, M. Comar, and R. Luzzati, “Measles: An overview of a re-emerging disease in children and immunocompromised patient,” Microorganisms, Vol.8, Issue 2, Article No.276, 2020. https://doi.org/10.3390/microorganisms8020276
- [31] G. E. C. Charnley, I. Kelman, K. A. M Gaythorpe, and K. A. Murray, “Traits and risk factors of post-disaster infectious disease outbreaks: a systematic review,” Scientific Reports, Vol.11, Article No.5616, 2021. https://doi.org/10.1038/s41598-021-85146-0
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.