Paper:
High-Dorsiflexion Assistive System for Passive Swing Phase Dorsiflexion Training and Preventing Compensatory Movements
Jing-Chen Hong*, Hiroki Ohashi**, and Hiroyasu Iwata***
*Graduate School of Creative Science and Engineering, Waseda University
3-4-1 Okubo, Shinjuku-ku, Tokyo 169-8555, Japan
**Department of Neurosurgery, Jikei University School of Medicine
3-25-8 Nishi-Shinbashi, Minato-ku, Tokyo 105-8461, Japan
***Faculty of Science and Engineering, Waseda University
3-4-1 Okubo, Shinjuku-ku, Tokyo 169-8555, Japan
Over the last few years, numerous robotic ankle-foot orthoses have been developed to help stroke patients optimize gait rehabilitation. In this paper, we present a study on the effects of assistance on dorsiflexion-restricted gait. Our high-dorsiflexion assistive system aims to provide full assistance to realize passive training of dorsiflexion during the swing phase and prevent compensatory movements. This system, which includes a McKibben-type artificial muscle and an air source, is lightweight and provides a high-dorsiflexion torque. The device could help boost overground gait rehabilitation in stroke patients. With this system, we conducted an experiment on five healthy participants whose dorsiflexion movements were restricted, and the extent of their compensatory movements differed. The results of the processed surface electromyography data differed significantly when dorsiflexion movement was assisted by our system. The spatial parameters also showed significantly improved compensatory movement inclination with sufficient assistance. These results indicate the potential of our system to assist in passive training of ankle dorsiflexion movements and to prevent incorrect gait in patients with low dorsiflexion abilities.
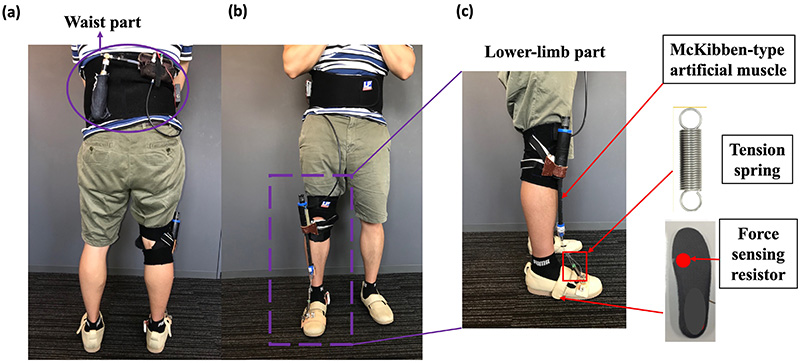
The appearance of the high-dorsiflexion assistive system
- [1] V. L. Feigin, G. A. Roth, M. Naghavi, P. Parmar, R. Krishnamurthi, S. Chugh, G. A. Mensah, B. Norrving, I. Shiue, M. Ng, and K. Estep, “Global burden of stroke and risk factors in 188 countries, during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013,” Lancet Neural., Vol.15, No.9, pp. 913-924, 2016.
- [2] N. Takashima, H. Arima, Y. Kita, T. Fujii, N. Miyamatsu, M. Komori, Y. Sugimoto, S. Nagata, K. Miura, and K. Nozaki, “Incidence, management and short-term outcome of stroke in a general population of 1.4 million Japanese-Shiga Stroke Registry,” Circ. J., Vol.81, No.11, pp.1636-1646, 2017.
- [3] M. Voigt and T. Sinkjaer, “Kinematic and kinetic analysis of the walking pattern in hemiplegic patients with drop foot using a peroneal nerve stimulator,” Clin. Biomech., Vol.15, No.5, pp. 340-351, 2000.
- [4] A. M. Wong, Y. C. Pei, W. H. Hong, C. Y. Chung, Y. C. Lau, and C. P. Chen, “Foot contact pattern analysis in hemiplegic stroke patients: an implication for neurologic status determination,” Arch. Phys. Med. Rehabil., Vol.85, No.10, pp. 1625-1630, 2004.
- [5] S. F. Tyson, E. Sadeghi-Demneh, and C. J. Nester, “A systematic review and meta-analysis of the effect of an ankle-foot orthosis on gait biomechanics after stroke,” Clin. Rehabil., Vol.27, No.10, pp. 879-891, 2013.
- [6] F. Alnajjar, R. Zaier, S. Khalid, and M. Gochoo, “Trends and Technologies in Rehabilitation of Foot Drop: A Systematic Review,” Expert Rev. Med. Devices, Vol.18, No.1, pp. 31-46, 2021.
- [7] B. Shi, X. Chen, X. Yue, X. Yin, Q. Weng, X. Zhang, J. Wang, and W. Wen, “Wearable ankle robots in post-stroke rehabilitation of gait: a systematic review,” Front. Neurorobot., Vol.13, No.63, pp. 1-16, 2019.
- [8] J. Bae et al., “A lightweight and efficient portable soft exosuit for paretic ankle assistance in walking after stroke,” Proc. IEEE Int. Conf. Robot. Autom., pp. 2820-2827, doi: 10.1109/ICRA.2018.8461046, 2018.
- [9] J. Kwon, J. H. Park, S. Ku, Y. Jeong, N. J. Paik, and Y. L. Park, “A Soft Wearable Robotic Ankle-Foot-Orthosis for Post-Stroke Patients,” IEEE Robot. Autom. Lett., Vol.4, No.3, pp. 2547-2552, 2019.
- [10] E. Tanaka, K. Muramatsu, K. Watanuki, S. Saegusa, and L. Yuge, “Development of a walking assistance apparatus for promotion of exercise,” Proc. IEEE Int. Conf. Robot. Autom., pp. 3711-3716, doi: 10.1109/ICRA.2016.7487557, 2016.
- [11] L. F. Yeung, C. Ockenfeld, M. K. Pang, H. W. Wai, O. Y. Soo, S. W. Li, and K. Y. Tong, “Randomized controlled trial of robot assisted gait training with dorsiflexion assistance on chronic stroke patients wearing ankle-foot orthosis,” J. Neuroeng. Rehabil., Vol.15, No.51, pp. 1-12, 2018.
- [12] J. E. Cho, J. S. Yoo, K. E. Kim, S. T. Cho, W. S. Jan, K. H. Cho, and W. H. Lee, “Systematic Review of appropriate robotic intervention for gait function in subacute stroke patients,” BioMed. Res. Int., Vol.2018, 4085298, 2018.
- [13] G. Moucheboeuf, R. Griffier, D. Gasq, B. Glize, L. Bouyer, P. Dehali, and H. Cassoudesalle, “Effects of robotic gait training after stroke: A meta analysis,” Ann. Phys. Rehabil. Med., Vol.63, pp. 518-534, 2020.
- [14] A. Wang, N. Hu, J. Yu, J. Lu, Y. Ge, and Y. Wang, “Human-Like Robust Adaptive PD Based Human Gait Tracking for Exoskeleton Robot,” J. Robot. Mechatron., Vol.33, No.1, pp. 88-96, 2021.
- [15] V. A. Stanhope, B. A. Knarr, D. S. Reisman, and J. S. Higginson, “Frontal plane compensatory strategies associated with self-selected walking speed in individuals post-stroke,” Clin. Biomech., Vol.29, No.5, pp. 518-522, 2014.
- [16] T. H. Cruz and Y. Y. Dhaher, “Impact of ankle-foot-orthosis on frontal plane behaviors post-stroke,” Gait Posture, Vol.30, No.3, pp. 312-316, 2009.
- [17] N. Roche, C. Bonnyaud, M. Geiger, B. Bussel, and D. Bensmail, “Relationship between hip flexion and ankle dorsiflexion during walking phase in chronic stroke patients,” Clin. Biomech., Vol.30, No.3, pp. 219-225, 2015.
- [18] R. A. Schimidt and C. A. Wrisberg, “Motor Learning and Performance: A Situation-Based Learning Approach,” 4th ed., Champaign, Illinoise: Human Kinematics, 2007.
- [19] H. Toda and S. Sugihara, “Ankle Joint Stretching Device Using Tension Rod for Self Rehabilitation,” J. Robot. Mechatron., Vol.33, No.4, pp. 843-850, 2021.
- [20] J. C. Hong, S. Suzuki, Y. Fukushima, K. Yasuda, H. Ohashi, and H. Iwata, “Development of High-Dorsiflexion Assistive Robotic Technology for Gait Rehabilitation,” Proc. IEEE Int. Conf. Syst. Man Cybern., pp. 3801-3806, doi: 10.1109/SMC.2018.00643, 2018.
- [21] J. C. Hong, G. Tanaka, K. Yasuda, H. Ohashi, and H. Iwata, “Identifying Spring Coefficient for Assisting Hemiplegic Patient’s Heel Rocker Function: A Feasibility Study,” Proc. IEEE Int. Conf. on Systems, Man, and Cybernetics, pp. 738-743, doi: 10.1109/SMC42975.2020.9283251, 2020.
- [22] Research Institute of Human Engineering for Quality Life, “Japanese Body Size Data,” 1997.
- [23] J. Perry and J. Burnfield, “Gait Analysis, Normal and Pathological Function,” 2nd ed., Thorofare, NJ: SLACK Incorporated, 2010.
- [24] Z. Zhou, Y. Sun, N. Want, F. Gao, K. Wei, and Q. Wang, “Robot-assisted rehabilitation of ankle plantar flexors spasticity: a 3-month study with proprioceptive neuromuscular facilitation,” Front. Neurorobot., Vol.10, pp. 1-14, 2016.
- [25] D. Zanotto, Y. Akiyama, P. Stegall, and S. K. Agrawal, “Knee joint misalignment in exoskeletons for lower extremities: effects on user’s gait,” IEEE Trans. Robot., Vol.31, No.4, pp. 978-987, 2015.
- [26] T. R. Mao, W. L. Lo, Q. Lin, L. Li, X. Xiao, P. Raghavan, and D. F. Huang, “The effect of body weight support treadmill training on gait recovery, proximal lower limb motor pattern, and balance in patients with subacute stroke,” Biomed. Res. Int., Vol.2015, 175719, 2015.
- [27] M. A. M. Dzahir and S. Yamamoto, “Recent trends in lower-limb robotic rehabilitation orthosis: control scheme and strategy for pneumatic muscle actuated gait trainers,” Robotics, Vol.3, No.2, pp. 120-148, 2014.
- [28] C. D. M. Nikamp, M. S. H. Hobbelink, J. van der Palen, H. J. Hermens, J. S. Rietman, and J. H. Buurke, “A randomized controlled trial on providing ankle-foot orthoses in patients with (sub-)acute stroke: Short-term kinematic and spatiotemporal effects and effects of timing,” Gait Posture, Vol.55, pp. 15-22, 2017.
- [29] J. Boudarham, N. Roche, D. Pradon, C. Bonnyaud, D. Bensmail, and R. Zory, “Variations in Kinematics during Clinical Gait Analysis in Stroke Patients,” PLoS One, Vol.8, No.6, e66421, 2013.
- [30] G. Morone, M. Bragoni, M. Iosa, D. D. Angelis, V. Venturiero, P. Coiro, L. Pratesi, and S. Paolucci, “Who may benefit from robotic assisted gait training? a randomized clinical trial in patients with subacute stroke,” Neurorehabil. Neural. Repair., Vol.25, No.7, pp. 636-644, 2011.
- [31] S. H. Peurala, O. Airaksinen, P. Huuskonen, P. Jäkälä, M. Juhakoski, K. Sandell, I. M. Tarkka, and J. Sivenius, “Effects of intensive therapy using gait trainer or floor walking exercises early after stroke,” J. Rehabil. Med., Vol.41, No.3, pp. 166-173, 2009.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.