Paper:
Development and Clinical Evaluation of Bed with Standing-Up Function
Katsuhiro Manabe
Department of Tokyo Physical Therapy, Faculty of Medical Sciences, Teikyo University of Science
2-2-1 Senju-Sakuragi, Adachi-ku, Tokyo 120-0045, Japan
The risk of disuse syndrome caused by prolonged supine posture in hemiplegic stroke in- and outpatients has become a social problem. This study aimed to develop a new bed with a standing-up function, allowing medical caregivers and patients to freely take a standing position on the bed to reduce the amount of time spent in the supine position and to clarify its effectiveness through evaluation of its usability and clinical use. In addition to the Gatch function of the developed bed, it allows transition from a supine position to a chair-sitting or standing position on the bed, and from a standing position to walking action. In addition, as with the tilt table used for standing-position training, the bed’s tilt angle can be adjusted, reducing the load on the lower limbs and allowing appropriate rehabilitation to be carried out anytime, consequently reducing the burden of nursing care. The bed was developed with the cooperation of a specialized bed manufacturer and supported by public funds, and clinical evaluation was conducted after confirming its safety. We evaluated the physical and physiological functions of two hemiplegic patients after 4 weeks of standing training using a prototype bed, to which results from the six-item test showed no significant improvement. However, medical professionals, such as doctors, nurses, and physical therapists, who participated in the clinical evaluation indicated that the bed can safely replace the tilt table for standing-position rehabilitation, and it is effective in eliminating related human and time burdens.
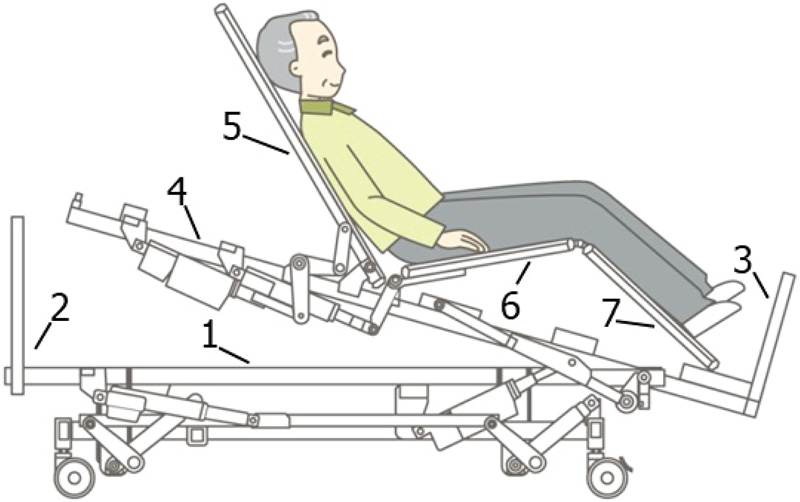
Mechanism of the 3D standing-up bed
- [1] J. E. Greenleaf, “Physiologic responses to prolonged bed rest and fluid immersion in humans,” J. Appl. Phsiol., Vol.57, pp. 619-633, 1984.
- [2] M. A. Perhonen, F. Franco, L. D. Lane et al., “Cardiac atrophy after bed rest and spaceflight,” J. Appl. physiol., Vol.91, pp. 645-653, 2001.
- [3] D. J. Glass, “Skeletal muscle hypertrophy and atrophy signaling pathways,” Int. J. Biochem. Cell Bio., Vol.37, pp. 1974-1984, 2005.
- [4] K. Takano, T. Watanabe, H. Suetsugu et al., “Nebulin and N-WASP cooperate to cause IGF-1-induced sarcomeric actin filament formation,” Science, Vol.330, No.6010, pp. 1536-1540, 2010.
- [5] R. Nakano, K. Hirasaka, J. Goto et al., “Ubiquitin ligase Cbl-b is a negative regulator for insulin-like growth factor 1 signaling during muscle atrophy caused by unloading,” Mol. Cell Biol., Vol.29, pp. 4798-4811, 2009.
- [6] M. R. Forward and D. B. Burr, “Physical activity and bone mass exercise in futilely?,” Bone Miner, Vol.21, pp. 89-112, 1993.
- [7] H. Sasaki, K. Manabe et al., “Report on the actual condition of disuse syndrome and corresponding equipment,” Japan Society for the Promotion of Industrial Technology, Research Committee for Development of Devices for Disuse Syndrome, 1999.
- [8] K. Manabe et al., “Validity of measuring the Physical Activity Time of Elderly Hemiplegics by an Activity Monitoring Evaluation System,” Rigakuryoho Kagaku, Vol.28, No.4, pp. 477-480, 2013.
- [9] K. Manabe, T. Hashizume et al., “Evaluation of daytime activities at home for elderly hemiplegic patients and development of bed with standing up function to prevent disuse syndrome,” Proc. of the 15th Int. Conf. on AAATE, 2019.
- [10] A. Tomono and H. Hiramatsu, “Stand-up training machine,” Application Number: (1993)63011.1993.2.26.
- [11] M. Takahashi, “Stand up training bed,” Application Number: (1994)146811.1994.6.28, 1994.
- [12] K. Ibe, “Stand up training bed for the Physically Challenged,” Application Number: (1995)27406.1995.1.23, 1995.
- [13] T. Hasegawa, “Bed equipment,” Application Number: (1993)148053.1993.6.18, 1993.
- [14] T. Sato, “Undulation bed,” Application Number: (1995)27026.1995.2.15, 1995.
- [15] T. Sakai, “Sitting up bed,” Application Number: (1995)145572.1995.5.18, 1995.
- [16] S. Annaka, “Raised bed,” Application Number: (1996)196606.1996.7.25, 1996.
- [17] T. Takeo, M. Nakano, and K. Manabe, “Sleeping platform,” Application Number: (1998)302645.1998.10.23, 1998.
- [18] Y. Kawakami, H. Akima, K. Kubo et al., “Changes in muscle size, architecture, and neural activation after 20 days of bed rest with and without resistance exercise,” Eur. J. Appl. Physiol. Occup. Physiol., Vol.84, pp. 7-12, 2001.
- [19] N. Brooks, G. Cloutier, S. Cadena et al., “Resistance training and timed essential amino acids protect against the loss of muscle mass and strength during 28 days of bed rest and energy deficit,” J. Appl. Physiol., Vol.105, pp. 241-248, 2008.
- [20] E. A. Muller, “Influence of training and of inactivity on muscle strength,” Arch. Phys. Med. Rhab., Vol.72, pp. 30-44, 2006.
- [21] H. Akima, “Resistance training during unweighting maintains muscle size and function in human calf,” Medicine & Science in Sports & Exercise, Vol.35, pp. 655-662, 2003.
- [22] H. Wakabayashi and H. Sashika, “Association of nutrition status and rehabilitation outcome in the disuse syndrome a retrospective cohort study,” General Medicine, Vol.12, pp. 69-74, 2011.
- [23] H. Wakabayashi and H. Sashika, “Malnutrition is associated with poor rehabilitation outcome in elderly inpatients with hospital-associated deconditioning a prospective cohort study,” J. Rehabil. Med., Vol.46, No.3, pp. 277-282, 2014.
- [24] A. Logan et al., “Standing Practice In Rehabilitation Early after Stroke (SPIRES): a functional standing frame program (prolonged standing and repeated sit to stand) to improve function and quality of life and reduce neuromuscular impairment in people with severe sub-acute stroke-a protocol for a feasibility randomised controlled trial,” Pilot and Feasibility Studies, Vol.4, pp. 1-18, 2018.
- [25] L. I. E. Oddsson et al., “Feasibility of early functional rehabilitation in acute stroke survivors using the Balance-Bed a technology that emulates microgravity,” Frontiers in Systems Neuroscience, Vol.9, 83, 2015.
- [26] M. Kawakami, S. Toba, K. Fukuda, S. Hori, Y. Abe, and K. Ozaki, “Application of Deep Learning to Develop a Safety Confirmation System for the Elderly in a Nursing Home,” J. Robot. Mechatron., Vol.29, No.2, pp. 338-345, 2017.
- [27] M. Nakamura, Y. Kume, J. Suzurikawa, S. Tsukada, H. Kawakami, K. Inoue, and T. Inoue, “Development of Transfer Assist Robot Based on the User Needs,” J. Robot. Mechatron., Vol.25, No.6, pp. 992-999, 2013.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.