Paper:
Effects of Gait Inducing Assist for Patients with Parkinson’s Disease on Double Support Phase During Gait
Ai Higuchi*1, Junichiro Shiraishi*2, Yuichi Kurita*3,*4, and Tomohiro Shibata*1
*1Graduate School of Life Science and Systems Engineering, Kyushu Institute of Technology
2-4 Hibikino, Wakamatsu-ku, Kitakyushu, Fukuoka 808-0196, Japan
*2University of Occupational and Environmental Health
1-1 Iseigaoka, Yahatanishi-ku, Kitakyushu, Fukuoka 807-8555, Japan
*3Graduate School of Engineering, Hiroshima University
1-4-1 Kagamiyama, Higashi-hiroshima, Hiroshima 739-8527, Japan
*4JST PRESTO
7 Gobancho, Chiyoda-ku, Tokyo 102-0076, Japan
Parkinson’s disease (PD) is a common progressive neurodegenerative disease that affects a wide range of motor and non-motor symptoms. Freezing of gait (FOG) is such a motor symptom of PD that frequently results in falling, and almost half of PD patients suffer from FOG. In this study, we investigated the effectiveness of a robotic assistance system called UPS-PD, which was developed to suppress FOG. The double limb support phase (DLS) in a 10-m straight-line walking task, the gait time and step counts were measured in five PD subjects. In addition, the safety of the UPS-PD in a healthy person was investigated using OpenSim, and the DLS parameters in four healthy elderly subjects were evaluated. In the experiment with the PD patients, the DLS parameters of two subjects showed an improvement. Furthermore, the step length of one subject and the step length and walking speed of the other subject were improved. Moreover, there were no problems in terms of instability of gait in both the PD patients. The UPS-PD did not adversely affect the gait of healthy elderly subjects and the walking of a healthy subject model in the simulation. Therefore, the UPS-PD is considered to be a useful device for improving walking in PD patients.
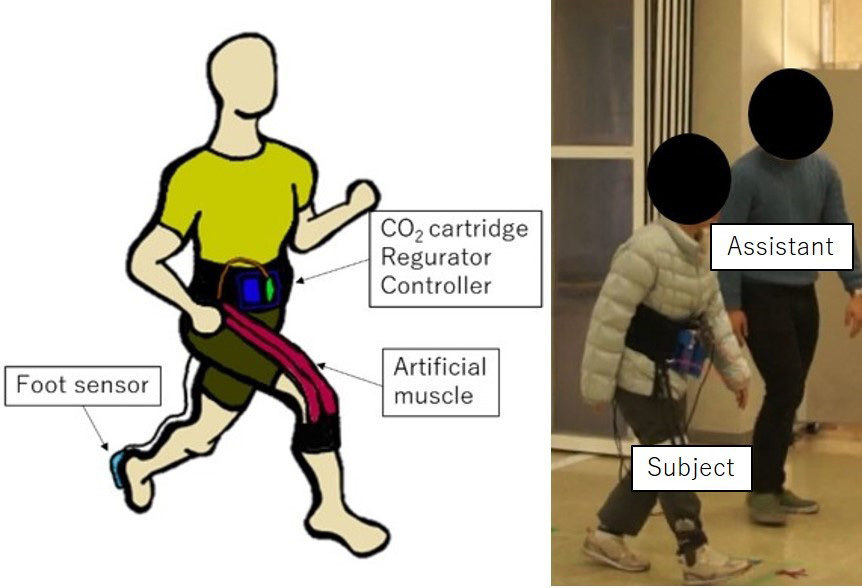
UPS-PD and an experiment
- [1] S. Kuzuhara, “Special Lecture 1 Current status and outlook of Parkinson’s disease treatment,” Clinical Neurology, Vol.48, No.11, pp. 835-843, 2008 (in Japanese).
- [2] P. Meir, G. Nir et al., “Is freezing of gait in Parkinson’s disease related to asymmetric motor function?,” Annals of Neurology: Official J. of the American Neurological Association and the Child Neurology Society, Vol.57, No.5, pp. 656-663, 2005.
- [3] M. Amboni, F. Stocchi et al., “Prevalence and associated features of self-reported freezing of gait in Parkinson disease: the DEEP FOG study,” Parkinsonism & Related Disorders, Vol.21, No.6, pp. 644-649, 2015.
- [4] Y. Okada, M. Osumi et al., “Examination of Factors Associated with Reduced Standard Wheelchair Driving Capacity in PD,” The J. of Movement Disorder and Disability, Vol.26, pp. 43-48, 2016 (in Japanese).
- [5] H. Kushida, K. Sawada et al., “Pedaling exercise using a foot-peddling wheelchair and its potential for rehabilitation of Parkinson’s disease,” J. of Rehabilitation Neurosciences, Vol.13, pp. 49-51, 2013 (in Japanese).
- [6] A. Fasano, C. Schlenstedt et al., “Split-belt locomotion in Parkinson’s disease links asymmetry, dyscoordination and sequence effect,” Gait & Posture, Vol.48, pp. 6-12, 2016.
- [7] R. Chee, A. Murphy et al., “Gait freezing in Parkinson’s disease and the stride length sequence effect interaction,” Brain, Vol.132, No.8, pp. 2151-2160, 2009.
- [8] A. Higuchi, T. Shibata et al., “A Study of the Release of Freezing of Gait in Parkinson’s Disease Patients Using Unplugged Powered Suits,” Proc. of JSME Conf. on Robotics and Mechatronics (Robomech) 2018, 2A2-G03, 2018 (in Japanese).
- [9] M. M. Hoehn, M. D. Yahr et al., “Parkinsonism: onset, progression, and mortality,” Neurology, Vol.17, No.5, pp. 427-442, 1967.
- [10] A. Higuchi, Y. Kurita et al., “Effects of UPS-PD on Gait in Patients With Parkinson’s Disease,” Proc. of the 36th Annual Conf. of the Robotics Society of Japan, 3A3-03, 2018 (in Japanese).
- [11] A. Higuchi, J. Shiraishi et al., “Gait Evaluation on Parkinson’s Disease Patients Using Spontaneous Stimulus Induced by UPS-PD,” Proc. of the 2019 IEEE/SICE Int. Symp. on System Integration, pp. 412-416, 2019.
- [12] P. Knobl, L. Kielstra, and Q. Almeida, “The relationship between motor planning and freezing of gait in Parkinson’s disease,” J. Neurol. Neurosurg. Psychiatry, Vol.83, No.1, pp. 98-101, 2012.
- [13] J. Verghese, R. Holtzer et al., “Quantitative gait markers and incident fall risk in older adults,” The J. of Gerontology: Series A, Vol.64, No.8, pp. 896-901, 2009.
- [14] K. Ogawa, C. Thakur et al., “Development of a pneumatic artificial muscle driven by low pressure and its application to the unplugged powered suit,” Advanced Robotics, Vol.31, No.21, pp. 1135-1143, 2017.
- [15] R. Baltadjieva, N. Giladi et al., “Marked alterations in the gait timing and rhythmicity of patients with de novo Parkinson’s disease,” European J. of Neuroscience, Vol.24, No.6, pp. 1815-1820, 2006.
- [16] S. L. Delp, F. C. Anderson et al., “OpenSim: open-source software to create and analyze dynamic simulations of movement,” IEEE Trans. on Biomedical Engineering, Vol.54, No.11, pp. 1940-1950, 2007.
- [17] L. Scott, J. Delp et al., “An interactive graphicsbased model of the lower extremity to study orthopaedic surgical procedures,” IEEE Trans. on Biomedical Engineering, Vol.37, pp. 757-767, 1990.
- [18] P. A. Rocha, G. M. Porfírio et al., “Effects of external cues on gait parameters of Parkinson’s disease patients: a systematic review,” Clinical neurology and neurosurgery, Vol.124, pp. 127-134, 2014.
- [19] M. S. Bryant, D. H. Rintala et al., “Gait variability in Parkinson’s disease: influence of walking speed and dopaminergic treatment,” Neurological Research, Vol.33, No.9, pp. 959-964, 2011.
- [20] E. Sejdić, Y. Fu et al., “The effects of rhythmic sensory cues on the temporal dynamics of human gait,” PLOS ONE, Vol.7, No.8, 2012.
- [21] M. F. del Olmo and J. Cudeiro, “Temporal variability of gait in Parkinson disease: Effects of a rehabilitation programme based on rhythmic sound cues,” Parkinsonism & Related Disorders, Vol.11, No.1, pp. 25-33, 2005.
- [22] M. Eto and A. Kubota, “Physical and Psychological Factors Affecting Falls in Healthy Elderly People at Home,” J. of Japan Society of Nursing Research, Vol.23, No.4, pp. 43-58, 2000 (in Japanese).
- [23] J. M. Bond and M. Morris, “Goal-directed secondary motor tasks: their effects on gait in subjects with Parkinson disease,” Archives of Physical Medicine and Rehabilitation, Vol.81, No.1, pp. 110-116, 2000.
- [24] K. Baker, L. Rochester, and A. Nieuwboer, “The immediate effect of attentional, auditory, and a combined cue strategy on gait during single and dual tasks in Parkinson’s disease,” Archives of Physical Medicine and Rehabilitation, Vol.88, No.12, pp. 1593-1600, 2007.
- [25] L. Rochester, A. Nieuwboer, K. Baker et al., “The attentional cost of external rhythmical cues and their impact on gait in Parkinson’s disease: effect of cue modality and task complexity,” J. of Neural Transmission, Vol.114, No.10, pp. 1243-1248, 2007.
- [26] M. Iosa, A. Fusco et al., “The golden ratio of gait harmony: repetitive proportions of repetitive gait phases,” BioMed Research Int., 2013.
- [27] I. Aprile, M. Galli et al., “Does first ray amputation in diabetic patients influence gait and quality of life?,” The J. of Foot and Ankle Surgery, Vol.57, No.1, pp. 44-51, 2018.
- [28] T. Miyake, Y. Kobayashi, M. Fujie, and S. Sugano, “One-DOF Wire-Driven Robot Assisting Both Hip and Knee Flexion Motion,” J. Robot. Mechatron., Vol.31, No.1, pp. 135-142, 2019.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.