Paper:
Training System for Endoscopic Surgery Aiming to Provide the Sensation of Forceps Operation
Tatsushi Tokuyasu*, Kumiko Motodoi*, Yuichi Endo**, Yukio Iwashita**, Tsuyoshi Etoh**, and Masafumi Inomata**
*Fukuoka Institute of Technology
3-30-1 Wajiro-higashi, Higashi-ku, Fukuoka 811-0295, Japan
**Oita University
1-1 Idaigaoka, Hasama-machi, Yufu City, Oita 879-5593, Japan
In Japan, a rising number of endoscopic surgery operations have boosted an expectation for the development of a training environment for qualified surgeons. The endoscopic surgery operation requires the operator to operate forceps by hand based on two-dimensional operative field information displayed on the monitor. The characteristics of the operation include a lack of stereoscopic visual field information and movement of the tip of the forceps, which is symmetric about the trocar. These are issues that require an empirical solution from the operator. It is desirable that these issues have already been overcome before the operator starts practicing as an operating surgeon. To this end, it is effective to train the operator in the sensation of forceps operation, which associates the operative field vision with the forceps operation by hand. Therefore, this study includes digitizing the forceps operation by qualified surgeons and providing it to the trainee as visual and force information in order to build a training device that facilitates the cultivation of the sensation of forceps operation.
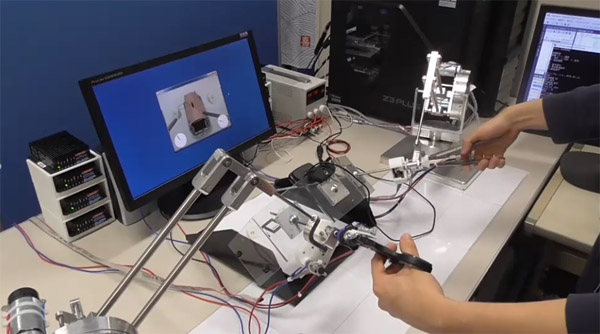
Training system for endoscopic surgery
- [1] H. Clarke, “Laparoscopy-New instruments for suturing and ligation,” Fertility and Sterility, Vol.23, No.4, pp. 274-277, 1972.
- [2] C. Alfred, “Whither minimal access surgery: tribulations and expectations,” The American J. of Surgery, Vol.169, Issue 1, pp. 9-19, 1995.
- [3] A. Moreno-Egea, J. A. Torralba-Martinez, G. Morales, T. Fernández, E. Girela, and J. L. Aguayo-Albasini, “Open vs laparoscopic repair of secondary lumbar hernias: a prospective nonrandomized study,” Surgical Endoscopy and Other Interventional Techniques, Vol.19, Issue 2, pp. 184-187, 2005.
- [4] G. Dedemadi, G. Sgourakis, C. Karaliotas, T. Christofides, G. Kouraklis, and C. Karaliotas, “Comparison of laparoscopic and open tension-free repair of recurrent inguinal hernias: a prospective randomized study,” Surgical Endoscopy and Other Interventional Techniques, Vol.20, Issue 7, pp. 1099-1104, 2006.
- [5] I. Murasawa, S. Murofushi, C. Ishii, and H. Kawamura, “Development of a Robotic Laparoscope for Laparoscopic Surgery and its Control,” J. Robot. Mechatron., Vol.29, No.3, pp. 580-590, 2017.
- [6] K. Takikawa, R. Miyazaki, T. Kanno, G. Endo, and K. Kawashima, “Pneumatically Driven Multi-DOF Surgical Forceps Manipulator with a Bending Joint Mechanism Using Elastic Bodies,” J. Robot. Mechatron., Vol.28, No.4, pp. 559-567, 2016.
- [7] Y. Sekiguchi, Y. Kobayashi, Y. Tomono, H. Watanabe, K. Toyoda, K. Konishi, M. Tomikawa, S. Ieiri, K. Tanoue, M. Hashizume, and M. Fujie, “Development of a Tool Manipulator Driven by a Flexible Shaft for Single-Port Endoscopic Surgery,” J. Robot. Mechatron., Vol.23, No.6, pp. 1115-1124, 2011.
- [8] M. F. Szwerc, R. J. Landreneau, R. S. Santos, R. J. Keenan, and G. F. Murray, “Minithoracotomy combined with mechanically stapled bronchial and vascular ligation for anatomical lung resection,” The Annals of Thoracic Surgery, Vol.77, Issue 6, pp. 1904-1910, 2004.
- [9] D. Y. Deng, M. V. Menga, H. T. Nguyen, G. C. Bellman, and M. L. Stoller, “Laparoscopic linear cutting stapler failure,” Urology, Vol.60, Issue 3, pp. 415-419, 2002.
- [10] S. Yamaguchi, K. Konishi, T. Yasunaga, D. Yoshida, N. Kinjo, K. Kobayashi, S. Ieiri, K. Okazaki, H. Nakashima, K. Tanoue, Y. Maehara, and M. Hashizume, “Construct validity for eye-hand coordination skill on a virtual reality laparoscopic surgical simulator,” Surgical Endoscopy, Vol.21, Issue 12, pp. 2253-2257, 2007.
- [11] B. Wentink, “Eye-hand coordination in laparoscopy-an overview of experiments and supporting aids,” Minimally Invasive Therapy & Allied Technologies, Vol.10, No.3, pp. 155-162, 2009.
- [12] G. R. Wignall, J. D. Denstedt, G. M. Preminger, J. A. Cadeddu, M. S. Pearle, R. M. Sweet, and E. M. McDougall, “Surgical simulation: a urological perspective,” The J. of Urology, Vol.179, Issue 5, pp. 1690-1699, 2008.
- [13] D. J. Scott and G. L. Dunnington, “The new ACS/APDS skills curriculum: moving the learning curve out of the operating room,” J. of Gastrointestinal Surgery, Vol.12, Issue 2, pp. 213-221, 2008.
- [14] R. Aggarwal, K. Moorthy, and A. Darzi, “Laparoscopic skills training and assessment,” British J. of Surgery, Vol.91, No.12, pp. 1549-1558, 2004.
- [15] R. F. Velthoven and P. Hoffmann, “Methods for laparoscopic training using animal models,” Current Urology Reports, Vol.7, Issue 2, pp. 114-119, 2006.
- [16] A. G. Gallagher, A. B. Lederman, K. McGlade, R. M. Satava, and C. D. Smith, “Discriminative validity of the Minimally Invasive Surgical Trainer in Virtual Reality (MIST-VR) Using Criteria Levels Based on Expert Performance,” Surgical Endoscopy and Other Interventional Techniques, Vol.18, Issue 4, pp. 660-665, 2004.
- [17] K. Tanoue, S. Ieiri, K. Konishi, T. Yasunaga, K. Okazaki, S. Yamaguchi, D. Yoshida, Y. Kakeji, and M. Hashizume, “Effectiveness of endoscopic surgery training for medical students using a virtual reality simulator versus a box trainer: a randomized controlled trial,” Surgical Endoscopy, Vol.22, Issue 4, pp. 985-990, 2008.
- [18] N. J. Soper and G. M. Fried, “The fundamentals of laparoscopic surgery: its time has come,” Bulletin of the Americal College of Surgeons, Vol.93, No.9, pp. 30-32, 2008.
- [19] G. M. Fried, A. M. Derossis, J. Bothwell, and H. H. Sigman, “Comparison of laparoscopic performance in vivo with performance measured in a laparoscopic simulator,” Surgical Endoscopy, Vol.13, Issue 11, pp. 1077-1081, 1999.
- [20] J. Brewin, T. Nedas, B. Challacombe, O. Elhage, J. Keisu, and P. Dasgupta, “Face, content and construct validation of the first virtual reality laparoscopic nephrectomy simulator,” BJU Int., Vol.106, No.6, pp. 850-854, 2010.
- [21] D. Kondo, H. Iizuka, H. Ando, K. Obama, Y. Sakai, and T. Maeda, “Learning Effect of Laparoscopy Training System Using View-Sharing Technology and Verification for Practical Use,” Trans. of the Virtual Reality Society of Japan, Vol.18, No.4, pp. 487-496, 2013 (in Japanese).
- [22] M. Chang, K. Aoyama, M. Furukawa, K. Obama, Y. Sakai, T. Maeda, and H. Ando, “Effect of Stereoscopic Display System on Training of Laparoscopic Surgery for Needle Insertion Skill,” Trans. of the Virtual Reality Scoiety of Japan, Vol.20, No.4, pp. 299-309, 2015 (in Japanese).
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.