Paper:
Characterization of Postural Control in Post-Stroke Patients by Musculoskeletal Simulation
Kohei Kaminishi*1, Dongdong Li*2, Ryosuke Chiba*3, Kaoru Takakusaki*3, Masahiko Mukaino*4, and Jun Ota*1
*1Research into Artifacts, Center for Engineering (RACE), School of Engineering, The University of Tokyo
7-3-1 Hongo, Bunkyo-ku, Tokyo 113-8656, Japan
*2Department of Precision Engineering, School of Engineering, The University of Tokyo
7-3-1 Hongo, Bunkyo-ku, Tokyo 113-8656, Japan
*3Division of Neuroscience, Department of Physiology, Asahikawa Medical University
2-1-1-1 Midorigaoka-higashi, Asahikawa, Hokkaido 078-8510, Japan
*4Department of Rehabilitation Medicine, Hokkaido University Hospital
Kita 14, Nishi 5, Kita-ku, Sapporo, Hokkaido 060-8648, Japan
An association is observed between the standing sway posture and falls in patients with stroke; hence, it is important to study their standing balance. Although there are studies on the standing balance in stroke patients, differences in control have not been adequately investigated. This study aims to propose a method to characterize the postural sway in standing stroke patients using a mathematical model. A musculoskeletal model and neural controller model were used to simulate ten stroke patients (five patients with cerebral hemorrhages and five patients with cerebral infarctions) and eight young healthy participants, and their data were monitored during quiet standing. The model parameters were adjusted by focusing on the maximum-minimum difference in sway, which was considered important in a previous study, and sway speed, which is frequently used in the analysis. The adjusted model parameters were subjected to dimension reduction using non-negative matrix factorization. Consequently, the sway characteristics of stroke patients were expressed as the magnitude of gain parameters related to the extension of the entire body. The results of this study demonstrated the possibility of representing the characteristics of postural sway as model parameters in stroke patients using a mathematical model. This characterization could lead to the design of individualized rehabilitation systems in the future.
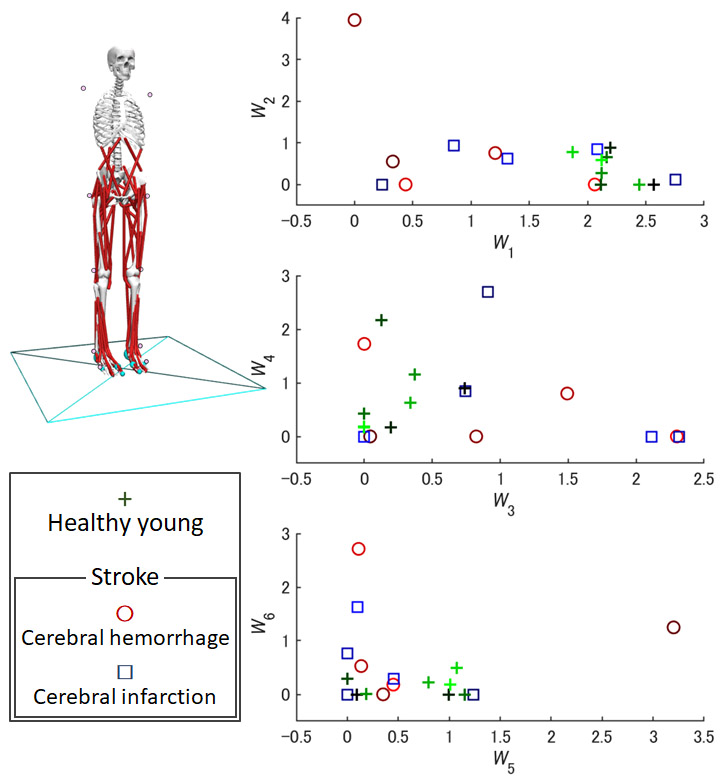
Extracted components of postural control
- [1] F. A. Batchelor, S. F. Mackintosh, C. M. Said, and K. D. Hill, “Falls after stroke,” Int. J. of Stroke, Vol.7, No.6, pp. 482-490, 2012.
- [2] C. M. Sackley, “Falls, sway, and symmetry of weight-bearing after stroke,” Int. disability studies, Vol.13, No.1, pp. 1-4, 1991.
- [3] J. Mizrahi, P. Solzi, H. Ring, and R. Nisell, “Postural stability in stroke patients: vectorial expression of asymmetry, sway activity and relative sequence of reactive forces,” Medical and Biological Engineering and Computing, Vol.27, No.2, pp. 181-190, 1989.
- [4] G. Rode, C. Tiliket, and D. Boisson, “Predominance of postural imbalance in left hemiparetic patients,” Scandinavian J. of Rehabilitation Medicine, Vol.29, No.1, pp. 11-16, 1997.
- [5] W. Wang, K. Li, N. Wei, C. Yin, and S. Yue, “Evaluation of postural instability in stroke patient during quiet standing,” 2017 39th Annual Int. Conf. of the IEEE Engineering in Medicine and Biology Society (EMBC), pp. 2522-2525, 2017.
- [6] Y. Asai, Y. Tasaka, K. Nomura, T. Nomura, M. Casadio, and P. Morasso, “A model of postural control in quiet standing: robust compensation of delay-induced instability using intermittent activation of feedback control,” PLoS One, Vol.4, No.7, Article No.e6169, 2009.
- [7] R. J. Peterka, “Sensorimotor integration in human postural control,” J. of Neurophysiology, Vol.88, No.3, pp. 1097-1118, 2002.
- [8] P. Jiang, R. Chiba, K. Takakusaki, and J. Ota, “Generation of the human biped stance by a neural controller able to compensate neurological time delay,” PLoS One, Vol.11, No.9, Article No.e0163212, 2016.
- [9] K. Kaminishi, P. Jiang, R. Chiba, K. Takakusaki, and J. Ota, “Postural control of a musculoskeletal model against multidirectional support surface translations,” PLoS One, Vol.14, No.3, Article No.e0212613, 2019.
- [10] A. D. Koelewijn and A. J. Ijspeert, “Exploring the Contribution of Proprioceptive Reflexes to Balance Control in Perturbed Standing,” Frontiers in Bioengineering and Biotechnology, Article No.866, 2020.
- [11] C. Maurer, T. Mergner, and R. Peterka, “Abnormal resonance behavior of the postural control loop in Parkinson’s disease,” Experimental Brain Research, Vol.157, No.3, pp. 369-376, 2004.
- [12] Y. Suzuki, A. Nakamura, M. Milosevic, K. Nomura, T. Tanahashi, T. Endo, S. Sakoda, P. Morasso, and T. Nomura, “Postural instability via a loss of intermittent control in elderly and patients with Parkinson’s disease: A model-based and data-driven approach,” Chaos: An Interdisciplinary J. of Nonlinear Science, Vol.30, No.11, Articel No.113140, 2020.
- [13] T. Yamamoto, Y. Suzuki, K. Nomura, T. Nomura, T. Tanahashi, K. Fukada, T. Endo, and S. Sakoda, “A classification of postural sway patterns during upright stance in healthy adults and patients with Parkinson’s disease,” J. Adv. Comput. Intell. Intell. Inform., Vol.15, No.8, pp. 997-1010, 2011.
- [14] F. Matsuda, M. Mukaino, K. Ohtsuka, H. Tanikawa, K. Tsuchiyama, T. Teranishi, Y. Kanada, H. Kagaya, and E. Saitoh, “Analysis of strategies used by hemiplegic stroke patients to achieve toe clearance,” Japanese J. of Comprehensive Rehabilitation Science, Vol.7, pp. 111-118, 2016.
- [15] S. L. Delp, F. C. Anderson, A. S. Arnold, P. Loan, A. Habib, C. T. John, E. Guendelman, and D. G. Thelen, “OpenSim: open-source software to create and analyze dynamic simulations of movement,” IEEE Trans. on Biomedical Engineering, Vol.54, No.11, pp. 1940-1950, 2007.
- [16] A. Seth, J. L. Hicks, T. K. Uchida, A. Habib, C. L. Dembia, J. J. Dunne, C. F. Ong, M. S. DeMers, A. Rajagopal, M. Millard et al., “OpenSim: Simulating musculoskeletal dynamics and neuromuscular control to study human and animal movement,” PLoS Computational Biology, Vol.14, No.7, Artile No.e1006223, 2018.
- [17] K. Kaminishi, R. Chiba, K. Takakusaki, and J. Ota, “Increase in muscle tone promotes the use of ankle strategies during perturbed stance,” Gait & Posture, Vol.90, pp. 67-72, 2021.
- [18] M. Millard, T. Uchida, A. Seth, and S. L. Delp, “Flexing computational muscle: modeling and simulation of musculotendon dynamics,” J. of Biomechanical Engineering, Vol.135, No.2, 2013.
- [19] K. H. Hunt and F. R. E. Crossley, “Coefficient of restitution interpreted as damping in vibroimpact,” J. of Applied Mechanics, Vol.42, No.2, 1975.
- [20] K. Takakusaki, R. Chiba, T. Nozu, and T. Okumura, “Brainstem control of locomotion and muscle tone with special reference to the role of the mesopontine tegmentum and medullary reticulospinal systems,” J. of Neural Transmission, Vol.123, No.7, pp. 695-729, 2016.
- [21] D. Li, K. Kaminishi, R. Chiba, K. Takakusaki, M. Mukaino, and J. Ota, “Evaluating quiet standing posture of post-stroke patients by classifying cerebral infarction and cerebral hemorrhage patients,” Advanced Robotics, Vol.35, No.13-14, pp. 878-888, 2021.
- [22] D. Li, K. Kaminishi, R. Chiba, K. Takakusaki, M. Mukaino, and J. Ota, “Evaluation of Postural Sway in Post-Stroke Patients by Dynamic Time Warping Clustering,” Frontiers in Human Neuroscience, Article No.731677, 2021.
- [23] N. Hansen and A. Ostermeier, “Completely derandomized self-adaptation in evolution strategies,” Evolutionary Computation, Vol.9, No.2, pp. 159-195, 2001.
- [24] M. W. Berry, M. Browne, A. N. Langville, V. P. Pauca, and R. J. Plemmons, “Algorithms and applications for approximate nonnegative matrix factorization,” Computational Statistics & Data Analysis, Vol.52, No.1, pp. 155-173, 2007.
- [25] G. Torres-Oviedo, J. M. Macpherson, and L. H. Ting, “Muscle synergy organization is robust across a variety of postural perturbations,” J. of Neurophysiology, Vol.96, No.3, pp. 1530-1546, 2006.
- [26] S. Paolucci, G. Antonucci, M. G. Grasso, M. Bragoni, P. Coiro, D. De Angelis, F. R. Fusco, D. Morelli, V. Venturiero, E. Troisi et al., “Functional outcome of ischemic and hemorrhagic stroke patients after inpatient rehabilitation: a matched comparison,” Stroke, Vol.34, No.12, pp. 2861-2865, 2003.
- [27] J. Tutuarima, J. V. d. Meulen, R. De Haan, A. Van Straten, and M. Limburg, “Risk factors for falls of hospitalized stroke patients,” Stroke, Vol.28, No.2, pp. 297-301, 1997.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.