Paper:
Fabrication and Characterization of a Biodegradable Hollow Microneedle from Chitosan
Masato Suzuki, Tomokazu Takahashi, and Seiji Aoyagi
Kansai University
3-3-35 Yamate-cho, Suita, Osaka 564-8680, Japan
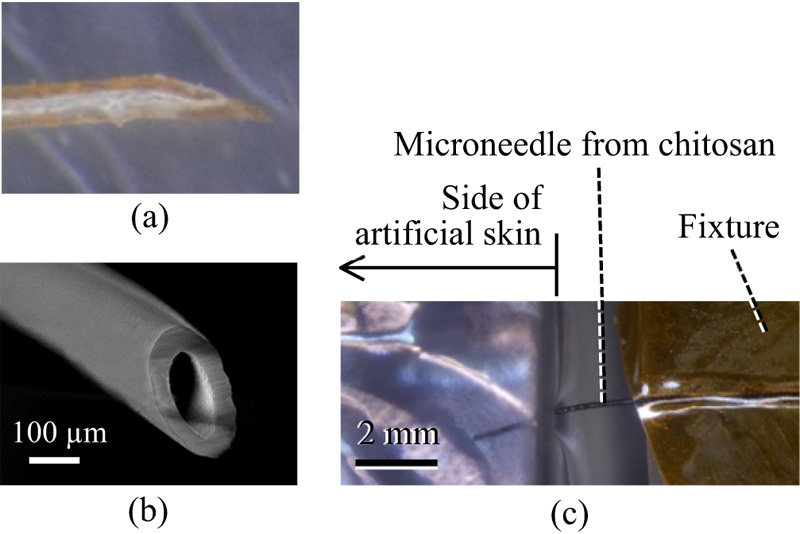
A biodegradable chitosan-acetate microneedle is developed based on the proboscis of a mosquito, which consists of chitin and protein. The formability of chitosan, which is a deacetylated compound of chitin, is improved by dissolving it in dilute acetic acid. Thereafter, the dissolved chitosan is coated around an Al wire by a dip-coating method, followed by drying. Afterward, the Al wire is removed by etching using an alkaline solution to form the chitosan micropipe. Subsequently, the micropipe is baked at 200°C for 0.20 min. The optimum baking time was found to be 17 min. Finally, the micropipe is cut and its tip sharpened to transform it into a microneedle with a length, an outer diameter, and an inner diameter of 4 mm, 150 μm, and 100 μm, respectively. The Young’s modulus of the fabricated chitosan microneedle is approximately 10 GPa. This microneedle could be inserted into an artificial skin made of silicone rubber without buckling, and it could aspirate blood from a frog at a rate of 2.5 μL/s.
Biodegradable hollow microneedle from chitosan
- [1] D. V. McAllister et al., “Microfabricated needles for transdermal delivery of macromolecules and nanoparticles: fabrication methods and transport studies,” Proc. Natl. Acad. Sci. U.S.A., Vol.100, pp. 13755-13760, 2003.
- [2] S. P. Davis, M. R. Prausnitz, and M. G. Allen, “Fabrication and characterization of laser micromachined hollow microneedles,” Proc. Transducers ’03, pp. 1435-1438, 2003.
- [3] M. R. Prausnitz, “Microneedles for transdermal drug delivery,” Advanced Drug Delivery Reviews, Vol.56, pp. 581-587, 2004.
- [4] H. Yagyu, S. Hayashi, and O. Tabata, “Fabrication of Plastic Micro Tip Array using Laser Micromachining of Nanoparticles Dispersed Polymer and Micromolding,” IEEJ Trans. on Sensors and Micromachines, Vol.126, pp. 7-13, 2006.
- [5] N. Roxhed, B. Samel, L. Nordquist, P. Griss, and G. Stemme, “Painless Drug Delivery Through Microneedle-Based Transdermal Patches Featuring Active Infusion,” IEEE Trans. on Biomedical Engineering, Vol.55, pp. 1063-1071, 2008.
- [6] K. Maaden, W. Jiskoot, and J. Bouwstra, “Microneedle technologies for (trans) dermal drug and vaccine delivery,” J. Control Release, Vol.161, pp. 645-655, 2012.
- [7] H. Izumi, M. Suzuki, S. Aoyagi, and T. Kanzaki, “Realistic Imitation of Mosquito’s Proboscis: Electrochemically etched Sharp and Jagged Needles and Their Cooperative Inserting Motion,” Sensors and Actuators A, Vol.165, No.1, pp. 115-123, 2011.
- [8] Y. Hara et al., “Fabrication of Stainless Steel Microneedle with Laser-Cut Sharp Tip and its Penetration and Blood Sampling Performance,” Int. J. Automation Technol., Vol.10, No.6, pp. 950-957, 2016.
- [9] T. Tanaka, T. Takahashi, M. Suzuki, and S. Aoyagi, “Development of Minimally Invasive Microneedle Made of Tungsten – Sharpening Through Electrochemical Etching and Hole Processing for Drawing up Liquid Using Excimer Laser,” J. Robot. Mechatron., Vol.25, pp. 755-761, 2013.
- [10] S. Aoyagi, H. Izumi, and M. Fukuda, “Biodegradable polymer needle with various tip angles and consideration on insertion mechanism of mosquito’s proboscis,” Sensors and Actuators A, Vol.143, pp. 20-28, 2008.
- [11] S. Aoyagi, H. Izumi, S. Nakahara, M. Ochi, and H. Ogawa, “Laser microfabrication of long thin holes on biodegradable polymer in vacuum for preventing clogginess and its application to blood collection,” Sensors and Actuators A, Vols.145-146, No.1, pp. 464-472, 2008.
- [12] M. Suzuki, T. Sawa, T. Takahashi, and S. Aoyagi, “Fabrication of Microneedle Mimicking Mosquito Proboscis Using Nanoscale 3D Laser Lithography System,” Int. J. Automation Technol., Vol.9, pp. 655-661, 2015.
- [13] M. Suzuki, T. Sawa, T. Takahashi, and S. Aoyagi, “Preparation of Biodegradable Chitosan Acetate Sheet and its Application to Microneedle,” Proc. Micro TAS 2014, pp. 1172-1174, 2014.
- [14] M.-C. Chen et al., “Chitosan Microneedle Patches for Sustained Transdermal Delivery of Macromolecules,” Biomacromolecules, Vol.13, pp. 4022-4031, 2012.
- [15] M.-C. Chen, S.-F. Huang, K.-Y. Lai, and M.-H. Ling, “Fully embeddable chitosan microneedles as a sustained release depot for intradermal vaccination,” Biomaterials, Vol.34, pp. 3077-3086, 2013.
- [16] L. E. Scriven, “Physics and applications of dip coating and spin coating,” Materials Research Society Symp. Proc., Vol.121, pp. 717-729, 1988.
- [17] J. H. Moon, G. R. Yi, and S. M. Yang, “Fabrication of hollow colloidal crystal cylinders and their inverted polymeric replicas,” J. Colloid and Interface Science, Vol.287, pp. 173-177, 2005.
- [18] S. E. Noriega and A. Subramanian, “Consequences of Neutralization on the Proliferation and Cytoskeletal Organization of Chondrocytes on Chitosan-Based Matrices,” Int. J. Carbohydrate Chemistry, Vol.2011, 809743, 2011.
- [19] K. Ogawa, “Effect of Heating an Aqueous Suspension of Chitosan on the Crystallinity and Polymorphs,” Agricultural and Biological Chemistry, Vol.55, pp. 2375-2379, 1991.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.