Paper:
Automated Femoral Stem Canal Fill Ratio Evaluation for Bipolar Hip Arthroplasty in 2D X-Ray Image
Yosuke Uozumi*, Kouki Nagamune**, and Keisuke Oe***
*Research Division on Advanced Information Technology, Cyberscience Center, Tohoku University
6-6-05 Aoba, Aramaki, Aoba-ku, Sendai, Miyagi 980-8579, Japan
**Department of Human and Artificial Intelligence Systems, Graduate School of Engineering, University of Fukui
3-9-1 Bunkyo, Fukui, Fukui 910-8507, Japan
***Department of Orthopaedic Surgery, Graduate School of Medicine, Kobe University
7-5-1 Kusunoki-Cho, Chuo-Ku, Kobe, Hyogo 650-0017, Japan
A stem loosening is one of the significant problem in the bipolar hip arthroplasty (BHA), causes a pain and instability of a patient’s hip, and requires a further surgery of BHA. A stem canal fill ratio (SCFR), a general evaluation of the stem loosening, have been clinically studied many; however, a determination of the optimal SCFR evaluation has not been still understood well. A purpose of this study is to propose an automatic and quantitative evaluation of SCFR from BHA hip X-ray image. A proposed method segmented the femoral canal and stem, and evaluated SCFR. In experiments, a proposed method’s accuracy was validated, and six BHA patients’ SCFRs were clinically evaluated (age 88±7 (74–93), one male / five females). In result of the proposed method’s accuracy, the femur canal was 90.60±3.65%, and the stem was 97.83±0.46%; therefore, the proposed method had the accuracy to well evaluate SCFR. Result of six BHA patients’ SCFRs was 63.70±5.62%. In conclusion, the proposed method was able to automatically evaluate SCFR from the hip X-ray image with BHA.
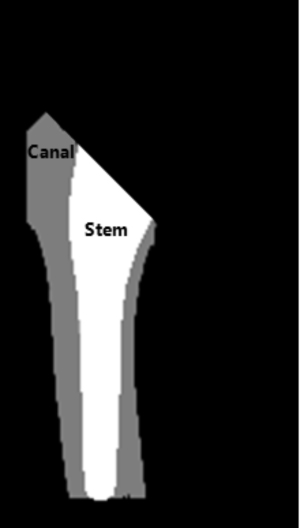
Femur canal fill ratio calculated by regions of canal and stem.
- [1] T. Visuri, T. Lindholm, I. Antti-Poika, and M. Koskenvuo, “The role of overlength of the leg in aseptic loosening after total hip arthroplasty,” Italian J. of Orthopaedics and Traumatology, Vol.19, No.1, pp. 107-111, 1992.
- [2] J. Dowd, L. Schwendeman, W. Macaulay, J. Doyle, A. Shanbhag, S. Wilson, J. Herndon, and H. Rubash, “Aseptic loosening in uncemented total hip arthroplasty in a canine model,” Clinical Orthopaedics and Related Research, Vol.319, pp. 106-121, 1995.
- [3] C. G. Mohler, J. J. Callaghan, D. K. Collis, and R. C. Johnston, “Early loosening of the femoral component at the cement-prosthesis interface after total hip replacement,” The J. of Bone & Joint Surgery, Vol.77, No.9, pp. 1315-1322, 1995.
- [4] E. Morscher and A. Schmassmann, “Failures of total hip arthroplasty and probable incidence of revision surgery in the future,” Archives of Orthopaedic and Traumatic Surgery, Vol.101, No.2, pp. 137-143, 1983.
- [5] W. H. Harris, “Advanced concepts in total hip replacement,” Slack, 1985.
- [6] C. Cyteval, M. P. Sarrabère, A. Cottin, C. Assi, L. Morcos, P. Maury, and P. Taourel, “Iliopsoas impingement on the acetabular component: radiologic and computed tomography findings of a rare hip prosthesis complication in eight cases,” J. of Computer Assisted Tomography, Vol.27, No.2, pp. 183-188, 2003.
- [7] H. J. Cooper, A. P. Jacob, and J. A. Rodriguez, “Distal fixation of proximally coated tapered stems may predispose to a failure of osteointegration,” The J. of Arthroplasty, Vol.26, No.6, pp. 78-83, 2011.
- [8] L. Dorr and C. Smith, “Clinical results from the calcitite-coated press fit APR hip system,” Dental Clinics of North America, Vol.36, No.1, pp. 239-246, 1992.
- [9] P. C. Noble, J. W. Alexander, L. J. Lindahl, D. T. Yew, W. M. Granberry, and H. S. Tullos, “The anatomic basis of femoral component design,” Clinical Orthopaedics and Related Research, Vol.235, pp. 148-165, 1988.
- [10] L. Spotorno and S. Romagnoli, “The CLS uncemented total hip replacement system,” 1991.
- [11] Y. Yeung, K. Chiu, W. Yau, W. Tang, W. Cheung, and T. Ng, “Assessment of the proximal femoral morphology using plain radiograph-can it predict the bone quality?,” The J. of Arthroplasty, Vol.21, No.4, pp. 508-513, 2006.
- [12] R. Brunelli, “Front Matter,” Wiley Online Library, 2009.
- [13] M. J. Parker, K. S. Gurusamy, and S. Azegami, “Arthroplasties (with and without bone cement) for proximal femoral fractures in adults,” The Cochrane Library, Vol.16, No.6, 2010.
- [14] C. K. Boese, B. Buecking, C. Bliemel, S. Ruchholtz, M. Frink, and P. Lechler, “The effect of osteoarthritis on functional outcome following hemiarthroplasty for femoral neck fracture: a prospective observational study,” BMC Musculoskeletal Disorders, Vol.16, No.1, p. 304, 2015.
- [15] Z. Zhou, F. Yan, W. Sha, L. Wang, and X. Zhang, “Unipolar Versus Bipolar Hemiarthroplasty for Displaced Femoral Neck Fractures in Elderly Patients,” Orthopedics, Vol.38, No.11, p. 697-702, 2015.
- [16] Y. Zhao, D. Fu, K. Chen, G. Li, Z. Cai, Y. Shi, and X. Yin, “Outcome of hemiarthroplasty and total hip replacement for active elderly patients with displaced femoral neck fractures: a meta-analysis of 8 randomized clinical trials,” Vol.9, No.5, p. e98071, 2014.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.